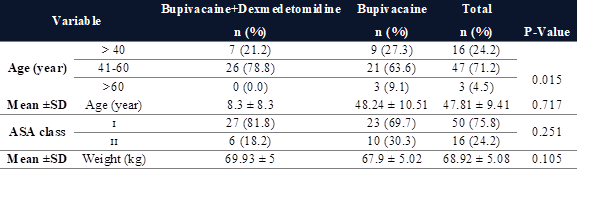
Table 1. Demographic characteristics of patients undergoing inguinal hernia
surgery in two groups through TAP block with ultrasound guide.
Ultrasound-guided
(USG) transversus abdominis plane (TAP) block with bupivacaine and
dexmedetomidine on the control in postoperative analgesia of inguinal hernia
surgery: A randomized clinical trial
Hossein Khoshrang 1, Hossein
Hemmati 2, Mohammad Reza Habibi 1*, Mohaya Farzin 3,
Abbas Sedighi-Nejad 4, Cyrus Emir Alavi 5, Zahra
Pourhabibi 6
1 Anesthesiology Research Center, Department of Anesthesiology,
Alzahra Hospital, Guilan University of Medical Sciences, Rasht, Iran
2 Department of Vascular Surgery, Razi Clinical Research Development
Unit, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran
3
Department of physiology, Razi Clinical Research Development Unit, Razi
Hospital, Guilan University of Medical Sciences, Rasht, Iran
4 Anesthesiology Research Center, Guilan University of Medical
Sciences, Rasht, Iran
5 Department of Anesthesiology, Neuroscience Research Center,
Avicenna University Hospital, Guilan University of Medical Sciences, Rasht,
Iran
6 Razi Clinical Research Development Unit, Razi Hospital, Guilan
University of Medical Sciences, Rasht, Iran
*Corresponding Author: Mohammad Reza
Habibi
* Email: mohammadreza.habibi.md@gmail.com
Abstract
Introduction: Transversus abdominis plane
block (TAPB) is now a well-established technique in postoperative analgesia for
lower abdominal surgeries. We aimed to investigate the effects of adding
dexmedetomidine to bupivacaine used in USG (TAP block on postoperative pain and
complications in patients undergoing inguinal hernia repair.
Materials
and Methods: About 66 eligible patients
enrolled in the survey. They were randomly assigned to one of the two groups of
20 CC of bupivacaine 0.5% + 1 CC Normal saline or 20 CC of bupivacaine 0.5% +
100µg dexmedetomidine. The amount of pethidine consumption, postoperative VAS
score, and complications were measured. Patients were evaluated at the recovery
ward (T0) and 2, 4, 6, 12, and 24 hours after surgery. Regarding the VAS score
and if the patient's pain complained from a VAS≥3, pethidine 0.5 mg/kg was
administered. The total dose, the average dose of pethidine used, and the first
time of pethidine administration after the nerve block was recorded.
Results: Two groups had no significant
difference regarding baseline characteristics. A significant difference was
found at T4 about VAS (P=0.005). The amount of pethidine consumption was lower
in the DEX group but not statistically significant except for T4 (P=0.006). The
two groups showed no difference regarding side effects such as PONV.
Conclusion: Injection of dexmedetomidine in combination with bupivacaine for TAPB
is an effective and safe drug for controlling pain after hernia surgery.
Keywords: Transversus abdominis plane
block; Bupivacaine; Dexmedetomidine; Inguinal hernia
Introduction
Hernia
repair surgery is one of the most common surgeries in the world pain is
one of the most common complications after hernia repair surgery. Chronic groin
pain has been reported to be about 6-10% in long-term follow-up (1,2). There are several causes of
postoperative pain. Include pain from incisions and deeper structures and
emotional pain, such as pain when coughing and moving. However, the central
pain is caused by an incision in the abdominal wall. Therefore, transversus
abdominis muscle block for postoperative pain in lower abdominal surgery,
including inguinal hernia, can be very effective, mainly when used as part of a
multi-modal analgesic regimen (3). Some methods have been used to
reduce postoperative pain. Drugs have been the gold standard for controlling
severe pain for many years, but the side effects of these drugs have always
posed challenges for physicians. These side effects include gastrointestinal
motility disorders, urinary retention, constipation, respiratory depression,
pruritus, abuse, postoperative vomiting nausea. Some other methods for
postoperative pain control include using Nonsteroidal anti-inflammatory drugs
(NSAIDs) and/or acetaminophen, gabapentin or pregabalin, I.V.
ketamine, epidural with local anesthetic (with or without opioid), or
intrathecal opioid, infusion of opioids with I.V.
patient-controlled analgesia (PCA) (4).
Abdominis
transversus muscle block has been used as an effective and safe method in
providing balance analgesia after abdominal surgery. Rafi first did this block
in 2001 (5). The abdominal transversus muscle
block creates a sensory block through local anesthetic infiltration between the
internal oblique and transverse abdominal muscles. In this block, three layers
of muscle, external oblique, internal oblique, and transverse abdominal muscle,
are anesthetized. Moreover, the T7–T12 intercostal muscles of the ilioinguinal
nerve, the iliohypogastric nerve, the L1–L3 nerves, and the lateral branches of
the cutaneous are blocked (6).
The
blocking reduces the use of drugs after surgery, the time of the first request
for pain relief, and the side effects of drugs. Among the available local
anesthetic drugs, long-acting types such as bupivacaine are an excellent
choice. Bupivacaine is an amide local anesthetic used in many studies to block (7). To perform this block, using an
ultrasound guide is more accurate and practical than blind methods (8,9). It also has fewer side effects
because the location of the needle and local anesthetic propagation is entirely
recognizable. However, performing this block without an ultrasound guide can
rupture the intraperitoneal membrane (10).
On
the other hand, in situations where only local anesthetics are used, one of the
problems with the block is the limitation of analgesia time. Other drugs as a
supplement to the block can increase the quality and time of the block effect
and reduce their side effects by decreasing the dose. Studies have shown the
addition of various drugs, including dexmedetomidine, morphine, sufentanil,
clonidine, adrenaline, and magnesium sulfate (11). Dexmedetomidine has been proposed
as an adjunct to local anesthetics. Many studies show that adding
dexmedetomidine to local anesthetics increases the duration of action and
analgesia time after surgery (12,13). It is a selective alpha two
receptor agonist that acts by inhibiting these receptors in the central nervous
system to inhibit the release of norepinephrine in a dose-dependent manner (14). It also reduces neuronal activity
through inhibitory effects on sodium and potassium channels and exerts its
analgesic role by inhibiting the transmission of neural messages in C-fibers.
The combination of bupivacaine and dexmedetomidine has been used successfully
in some other blocks (15,16).
Due to the importance of the issue and its
application in improving the quality of life of patients, providing desirable
medical services, and reducing hospitalization days and economic costs, we
decided to conduct the present study with the aim of the effectiveness of TAPB
with USG in reducing pain after inguinal hernia surgery in Razi Hospital,
Rasht, Iran.
Materials and Methods
Study
design and variables
This
study was a controlled, randomized clinical trial with a double-blind, parallel
design on patients who were candidates for elective inguinal hernia surgery. It
was performed with an age range of 18 to 65 years and with ASA class I, II.
After approving the draft study and receiving the ethical code
(IR.GUMS.REC.1397.449) and IRCT code (IRCT20121216011766N5), obtaining
informed consent from eligible patients was included. In addition, all
methods were performed following the Declaration
of Helsinki, and all individuals consented to participate in this study.
Patients who met the inclusion criteria were randomly assigned by one of the
nurses of the relevant ward who was unaware of the study to two groups of 33
people with Intervention (I) and control (C) marks in intervention and control groups. Random
sequences were generated using the Random Generator program. Based on the
randomized block method, 15 blocks of size 4 with a ratio of 1 to 1 (as two
groups I and C) and one block of six were generated for 66 patients. After
generating the list, each person was assigned a unique code, and during the
study, the person was identified with this code. All patients underwent general
anesthesia, and the patient's vital signs, including heart rate, respiration
rate, and blood pressure, were monitored and recorded. Immediately after the
operation and before transferring the patient to the recovery unit, by placing
the 15 MHz linear probe of the ultrasound device (Midray) in a transverse
position, just above the iliac crest and in the maxillary line on the same side
of the surgery, after finding the sheet between the internal oblique muscle and
the abdominal transversus muscle using ultrasound, in the control group: 20cc
of 0.5% bupivacaine with 1cc of normal saline, and intervention group: 20cc of
0.5% bupivacaine with 1cc (100 mcg) of dexmedetomidine were injected (brand
name Precedex containing 200 mcg/2ml, manufacturer HOSPIRA reference
manufacturer of USA).
In
the post-anesthesia care unit (PACU), at intervals of 0, 2, 4, 6, 12, and 24
hours after surgery, pain intensity was measured in two groups by VAS by asking
the patient to show their pain intensity on a 10 cm ruler. A score of zero was
given for analgesia, and a score of 10 for maximum pain. During the 24 hours,
the patients were hospitalized in the ward, 0.5 mg/kg of pethidine was
prescribed if they needed analgesia (VAS>3). The total dose, the average
dose of pethidine used, and the first time of pethidine administration after
the nerve block was recorded. Complications such as nausea, dizziness, and
vomiting in the two groups were evaluated. Inclusion criteria are age 18 to 65
years, body mass index 18-35 kg/m2, drug insensitivity, ASA Class I,
II, no infection at the injection site, no alcohol and drug addiction, and type
of surgery (Inguinal hernia repair without tension). Also, surgery lasting more
than two hours, the need for other operations during inguinal hernia surgery,
the requirement to receive drugs in recovery, excessive bleeding, recurrence of
hernias, and the need for spinal anesthesia excluded patients from the study.
Statistical
Analysis
The
required sample size was calculated using G*Power © software version 3.1.0.
About 26 patients in each group were estimated by assuming the test power of
80%, and the first type error was 0.05 to determine the effect size of 0.8 (17). Finally, 33 patients in each group
were determined by considering the 20% drop coefficient. The SPSS software
version 18 was used for all statistical analyses. Fisher and Chi-square tests
were used to compare the ratios in the two groups. Also, to compare the
quantitative means in the two groups, the Mann-Whitney U test, and to compare
the analgesia time, Kaplan-Meier and TaroneWare tests were used. Generalized
Linear Models (GLM) and Generalized Estimating Equation (GEE) were used to
investigate the effect of drugs on VAS scores during the study period. A value
of P< 0.05 was considered statistically significant
Results
Demographic
characteristics of patients undergoing inguinal hernia surgery in two groups
affected by bupivacaine injection and combined with dexmedetomidine via TAP
block with ultrasound guide were examined by chi-square test, which the results
are shown in Table 1. It was also found that in the C group, there was a
statistically significant difference between the values of VAS in the periods
studied (P<0.001). Also, there is a statistically significant difference
between the two groups between VAS values in the studied periods (P=0.047).
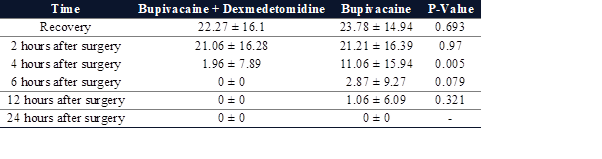
As shown in Table 2, intergroup statistical estimation illustrated that there
was a statistically significant difference between the amounts of pethidine
intake in bupivacaine+dexmedetomidine (F=44.86, P<0.001) and bupivacaine
groups (F=28.6, P<0.001). A significant difference was also found in the
statistical estimation between groups (F=3.89, P<0.001) according to the
period. The comparison between the mean of pethidine intake among two groups
with (45.3 ± 29.47) and without (60.0 ± 37.79) dexmedetomidine was not
statistically significant (P=0.094).
Table 1. Demographic characteristics of patients undergoing inguinal hernia
surgery in two groups through TAP block with ultrasound guide.
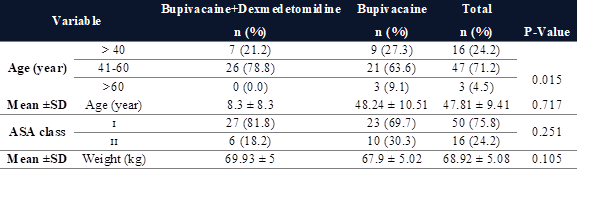
Table 2. Evaluation of changes in pethidine intake (mg) and comparison of
mean pethidine in patients undergoing inguinal
hernia surgery in two groups via TAP block.
Moreover,
the comparison of mean pethidine in patients in these two groups was shown that
no significant differences were found between the amounts of pethidine intake
(P=0.094) (Figure 1).
According to the information shown in Figure
2, using a t-test, it was found that only 4 hours after surgery, there was a
statistically significant difference between the amounts of pethidine in the
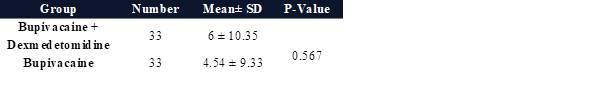
two groups (P=0.005). According to Mann-Whitney U test results in Table 3, a
significant difference was not observed between the values of analgesia
duration (hours) in patients in two groups 24 hours after surgery (P=0.567).
Table 3. Comparison of analgesia duration in patients
undergoing inguinal hernia surgery in two groups through TAP block in 24 hours
after surgery.
Based on Chi-square test results, table 4, a statistically
significant relationship was not observed between the incidence of side effects
(nausea or vomiting, or dizziness) in the two groups 24 hours after surgery
(P=0.459).
Table 4. Evaluation of side effects (nausea
or vomiting) in patients undergoing inguinal hernia surgery in two groups.
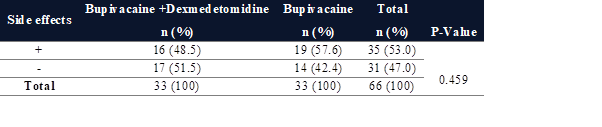
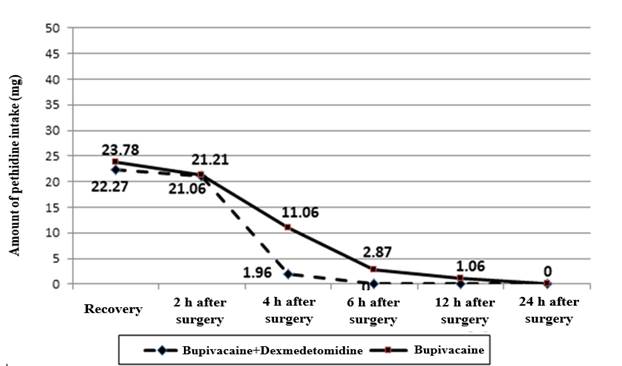
Figure 1. Evaluation of changes in pethidine
intake in patients undergoing inguinal hernia surgery in two groups under the
influence of bupivacaine injection alone and in combination with
dexmedetomidine via TAP block.
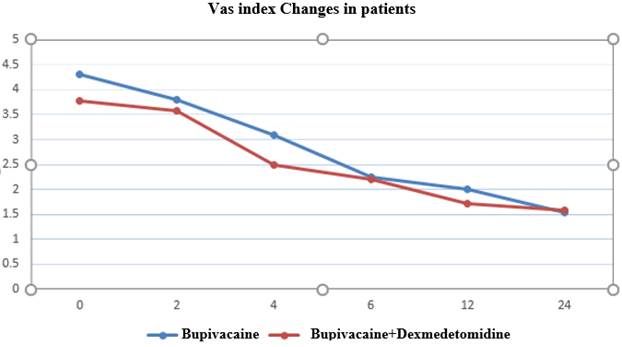
Figure 2. Evaluation of VAS index changes in
patients undergoing inguinal hernia surgery in two groups via TAP.
Discussion
Acute postoperative pain strongly predicted persistent pain
following both open anterior and endo-laparoscopic hernia repair (18). Physiological responses to
surgical pain and trauma include respiratory effects, cardiovascular,
Gastrointestinal, urinary system, neuroendocrine, and metabolic, which lead to
side effects. Control of physiological processes associated with acute
postoperative pain can lead to satisfaction and increase the quality of life in
patients (19). Kokoulu et al. described the block
as an effective and cost-effective method. Their study reported significantly
lower levels of anesthetic drugs in the group that underwent this block than in
the group undergoing standard general anesthesia and laparoscopic inguinal
hernia surgery (20).
Various methods have been proposed to control acute pain after
surgery, including administering nonsteroidal anti-inflammatory drugs,
peripheral nerve block, and nerve root block (21). Increasing awareness of
drug-related side effects, including respiratory depression, obstruction, and
sedation, has led to a shift in drug use to control postoperative pain (22). TAP block has been used as an
effective and safe method in providing balance analgesia after abdominal
surgery by blocking the abdominal wall nerve. In the USG method, local
anesthetics are injected near the nerve and help increase the injection's
accuracy (23). Various studies have shown that
TAP block is an effective technique for controlling pain and reducing morphine
use after surgery, including retropubic prostatectomy, colorectal surgery, a
cesarean delivery, abdominal hysterectomy, laparoscopic appendectomy, and
abdominal hernia surgery (23–26).
This study evaluated the effectiveness of TAP block with USG in
reducing pain after inguinal hernia surgery. It showed that the pain intensity
in the two groups significantly differed in the first four hours after surgery.
No significant difference in hemodynamic changes (H.R., MAP) was observed in
any of the cases during surgery. During the first four hours after surgery, a
significant difference was observed between the two groups regarding pethidine
consumption. However, in the following hours, between 4 and 12 hours, the
amount of pethidine in the two groups was not significantly different. In
addition, there was no significant difference between the two groups regarding
postoperative side effects.
According to other studies, analgesia time with bupivacaine block is
about 4-6 hours. Therefore, the results of this study can be justified that in
the first 4 hours, no significant difference was observed between the two
groups in terms of VAS score. However, after this time and with the
disappearance of bupivacaine effects, the effectiveness of dexmedetomidine
increased block efficiency. Furthermore, Aksu et al. reported the satisfaction
of patients who have undergone abdominal surgery (26). Therefore, the results of this
study are consistent with the present study and suggest that dexmedetomidine is
a drug whose addition to bupivacaine in TAP block reduces pain and drug use
after surgery. It should be noted that the dose of drugs used in the two
studies is the same.
In the study of Feyz et al.,
the pain of patients in resting and moving positions in the
ilioinguinal/iliohypogastric group was less than the TAP block group, which was
statistically significant. Besides, satisfaction with analgesia was
significantly higher in the ilioinguinal/iliohypogastric group than in the TAP
block group. Therefore, it was suggested that the iliohypogastric
ultrasound-guided block is more suitable than the TAP block; and to control
pain after inguinal hernia surgery, the ultrasound-guided ilioinguinal
/iliohypogastric block is more appropriate than the TAP block (27). In the current study, superiority
was not observed for the TAP block, which can be justified due to the
difference in the method of the present study with this study, which used
bupivacaine alone. Due to the high prevalence of this operation and its
increasing importance in controlling acute pain after surgery is a topic that
requires extensive research.
Limitations
Since the characteristics of people and their interpretation of
pain intensity, their expectation of pain, and their level of tolerance are
different and can be effective in expressing pain by the patient; it is
challenging to assess patients' pain. Furthermore, due to the limited follow-up
times, the evaluation of patients was limited in terms of possible
complications and the procedure's effectiveness.
Conclusions
According to the results of this
study, injection of dexmedetomidine in combination with bupivacaine for TAPB
can be used as an effective and safe drug for controlling pain after hernia
surgery.
Author contribution
HKH and HH researched literature and conceived the study. CEA
and ZP were involved in protocol development, gaining ethical approval,
patient recruitment and data analysis. MF, MRH and ASN wrote
the first draft of the manuscript. All authors reviewed and edited the
manuscript and approved the final version of the manuscript
Conflict of interest
The authors reported no potential conflict of interest.
Ethics approval
This study was approved by the ethical committee at the Guilan
University of Medical Sciences [I.R.GUMS.REC.1397.449].
References
1. Takebayashi K, Matsumura M, Kawai Y, Hoashi
T, Katsura N, Fukuda S, et al. Efficacy of transversus abdominis plane block
and rectus sheath block in laparoscopic
inguinal hernia surgery. Int Surg. April 2015;100(4):666–71.
2. Eklund A, Montgomery A,
Bergkvist L, Rudberg C. Chronic pain 5 years after randomized comparison of
laparoscopic and Lichtenstein inguinal
hernia repair. Br J Surg. April 2010;97(4):600–8.
3. Hutchins J, Delaney D,
Vogel RI, Ghebre RG, Downs LSJ, Carson L, et al. Ultrasound guided subcostal
transversus abdominis plane (TAP) infiltration with liposomal bupivacaine for patients undergoing
robotic assisted hysterectomy: A prospective randomized controlled study.
Gynecol Oncol. September 2015;138(3):609–13.
4. Chou R, Gordon DB, de
Leon-Casasola OA, Rosenberg JM, Bickler S, Brennan T, et al. Management of
Postoperative Pain: A Clinical Practice Guideline From the American Pain Society, the American Society of
Regional Anesthesia and Pain Medicine, and the American Society of
Anesthesiologists' Committee on Regional Anesthesia, Executive Committee, and
Administrative Council. J pain. Februarie 2016;17(2):131–57.
5. Tran DQ, Bravo D,
Leurcharusmee P, Neal JM. Transversus Abdominis Plane Block: A Narrative
Review. Anesthesiology. November 2019;131(5):1166–90.
6. Raof RA, El Metainy SA,
Alia DA, Wahab MA. Dexmedetomidine decreases the required amount of bupivacaine
for ultrasound-guided transversus
abdominis plane block in pediatrics patients: a randomized study. J Clin
Anesth. Februarie 2017;37:55–60.
7. Balakrishnan K,
Ebenezer V, Dakir A, Kumar S, Prakash D. Bupivacaine versus lignocaine as the
choice of locall anesthetic agent for
impacted third molar surgery a review. J Pharm Bioallied Sci. April
2015;7(Suppl 1):S230-3.
8. Fang WH, Chen XT,
Vangsness CTJ. Ultrasound-Guided Knee Injections Are More Accurate Than Blind
Injections: A Systematic Review of
Randomized Controlled Trials. Arthrosc Sport Med Rehabil. Augustus 2021;3(4):e1177–87.
9. McDermott G, Korba E,
Mata U, Jaigirdar M, Narayanan N, Boylan J, et al. Should we stop doing blind
transversus abdominis plane blocks? Br J Anaesth. Maart 2012;108(3):499–502.
10. Eslamian L, Kabiri-Nasab
M, Agha-Husseini M, Azimaraghi O, Barzin G, Movafegh A. Adding Sufentanil to
TAP Block Hyperbaric Bupivacaine Decreases Post-Cesarean Delivery Morphine Consumption. Acta Med Iran.
Maart 2016;54(3):185–90.
11. Rana S, Verma RK, Singh
J, Chaudhary SK, Chandel A. Magnesium sulphate as an adjuvant to bupivacaine in
ultrasound-guided transversus abdominis
plane block in patients scheduled for total abdominal hysterectomy under
subarachnoid block. Indian J Anaesth. Maart 2016;60(3):174–9.
12. Ding W, Li W, Zeng X, Li
J, Jiang J, Guo C, et al. Effect of Adding Dexmedetomidine to Ropivacaine on
Ultrasound-Guided Dual Transversus
Abdominis Plane Block after Gastrectomy. J Gastrointest Surg Off J Soc Surg Aliment Tract. Junie 2017;21(6):936–46.
13. Fritsch G, Danninger T,
Allerberger K, Tsodikov A, Felder TK, Kapeller M, et al. Dexmedetomidine added
to ropivacaine extends the duration of interscalene brachial plexus blocks for elective shoulder
surgery when compared with ropivacaine alone: a single-center, prospective,
triple-blind, randomized controlled trial. Reg Anesth Pain Med.
2014;39(1):37–47.
14. Knezevic NN,
Anantamongkol U, Candido KD. Perineural dexamethasone added to local anesthesia
for brachial plexus block improves pain
but delays block onset and motor blockade recovery. Pain Physician.
2015;18(1):1–14.
15. Tsantoulas C, McMahon
SB. Opening paths to novel analgesics: the role of potassium channels in
chronic pain. Trends Neurosci. Maart
2014;37(3):146–58.
16. Sun Q, Liu S, Wu H, Ma
H, Liu W, Fang M, et al. Dexmedetomidine as an Adjuvant to Local Anesthetics in
Transversus Abdominis Plane Block: A
Systematic Review and Meta-analysis. Clin J Pain. April 2019;35(4):375–84.
17. Hotujec BT, Spencer RJ,
Donnelly MJ, Bruggink SM, Rose SL, Al-Niaimi A, et al. Transversus abdominis
plane block in robotic gynecologic oncology: a randomized, placebo-controlled trial. Gynecol Oncol.
Maart 2015;136(3):460–5.
18. Olsson A, Sandblom G,
Franneby U, Sondén A, Gunnarsson U, Dahlstrand U. Do postoperative
complications correlate to chronic pain following inguinal hernia repair? A prospective cohort study
from the Swedish Hernia Register. Hernia. Februarie 2023;27(1):21–9.
19. Gousheh MR, Pipelzadeh
MR, Akhondzadeh MR, Olapour AR, Alizadeh Z, Sahafi SA. Intraoperative
Administration of Magnesium Sulfate on Postoperative Pain of Inguinal
Herniorrhaphy under General Anesthesia. Armaghane Danesh. 2013;18(6) :420–9.
20. Kokulu S, Bakı ED, Kaçar
E, Bal A, Şenay H, Üstün KD, et al. Effect of transversus abdominis plane block
on cost of laparoscopic cholecystectomy
anesthesia. Med Sci Monit Int Med J
Exp Clin Res. Desember 2014;20:2783–7.
21. Soleimani S, Saghafinia
M, Panahi Y, Madani SJ. Designing an evidence-based guideline for acute pain
management in orthopedic surgeries. Anesthesiol Pain. 2014;5(2):10–8.
22. Soliz JM, Lipski I,
Hancher-Hodges S, Speer BB, Popat K. Subcostal transverse abdominis plane block
for acute pain management: a review. Anesthesiol Pain Med. 2017;7(5).
23. Tsai H-C, Yoshida T,
Chuang T-Y, Yang S-F, Chang C-C, Yao H-Y, et al. Transversus abdominis plane
block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017.
24. Elkassabany N, Ahmed M,
Malkowicz SB, Heitjan DF, Isserman JA, Ochroch EA. Comparison between the
analgesic efficacy of transversus abdominis plane (TAP) block and placebo in open retropubic radical
prostatectomy: a prospective, randomized, double-blinded study. J Clin Anesth.
September 2013;25(6):459–65.
25. Favuzza J, Delaney CP.
Laparoscopic-guided transversus abdominis plane block for colorectal surgery.
Dis Colon Rectum. Maart 2013;56(3):389–91.
26. Mankikar MG, Sardesai
SP, Ghodki PS. Ultrasound-guided transversus abdominis plane block for
postoperative analgesia in patients
undergoing caesarean section. Indian J Anaesth. April 2016;60(4):253–7.
27. Faiz SHR, Nader ND,
Niknejadi S, Davari-Farid S, Hobika GG, Rahimzadeh P. A clinical trial
comparing ultrasound-guided ilioinguinal/iliohypogastric nerve block to transversus abdominis plane block
for analgesia following open inguinal hernia repair. J Pain Res. 2019;12:201–7.