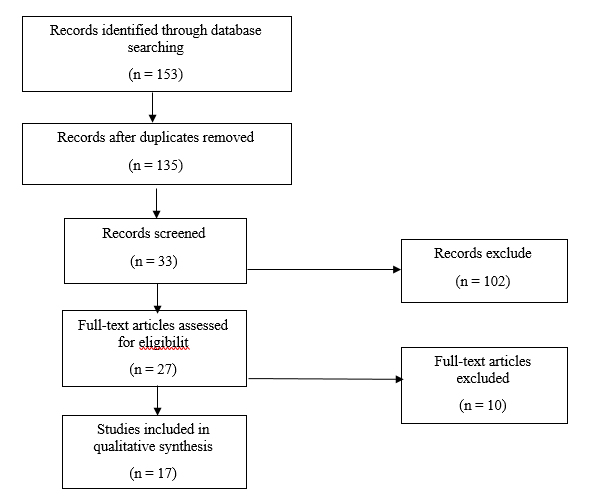
Figure 1. Flow diagram of the study selection for the review process.
The effect of
coronavirus pandemic on weight outcomes of patients after bariatric surgery
Seyyedeh Haniyeh Mousavibaghi 1*, Sedigheh Hannani 2
1 Department of Operating Room, Faculty of Paramedical Sciences, Guilan University of Medical Sciences, Rasht, Iran
2 Department of Operating Room, Faculty of Paramedical Sciences, Iran
University of Medical Sciences, Tehran, Iran
*Corresponding
Author: Seyyedeh Haniyeh Mousavibaghi
* Email: Haniyehmousavibaghi12@gmail.com
Abstract
Introduction: Coronavirus 2019 (COVID-19) was first reported in December 2019 in
Wuhan, China, and on January 30, 2020, the World Health Organization (WHO)
declared the outbreak of COVID-19 to be an international concern. Many
governments around the world quarantined and forced millions to stay at home
and remain isolated for long periods, an unprecedented impact on public life.
Patients who have undergone bariatric surgery are no exception but are more
vulnerable to the effects of isolation. This review study was conducted to help
to better understand the consequences of the COVID-19 virus pandemic on the
weight outcomes of patients after bariatric surgery.
Materials
and Methods: This review study examined the data from several reliable databases
such as Google Scholar, Scopus, and Science Direct from the beginning of the
coronavirus pandemic (2019) until now (2023). According to the inclusion
criteria, finally, 17 articles were reviewed.
Results: The findings of this study showed that increased psychological
distress, anxiety, depression and loneliness, mood changes, decreased physical
activity, decreased social support and loss of face-to-face meetings with a
nutrition consultant, increased substance use Unhealthy diet, increased
snacking and overeating, as well as loss of control over eating, are some of
the adverse effects of coronavirus pandemic on patients who have undergone
bariatric surgery, and these are risk factors for weight gain after bariatric
surgery.
Conclusion: Patients who have undergone bariatric surgery are affected by the
COVID-19 virus pandemic and subsequent quarantine and social isolation in many
areas of their lives, which will ultimately have a negative impact on the
weight outcomes of patients after surgery. Therefore, specialized care and
interventions are needed to address behaviors that lead to weight regain during
future pandemics or in the post-coronavirus era in vulnerable patients after
bariatric surgery.
Keywords: Coronavirus, Weight outcomes, Bariatric surgery
Introduction
Acute
respiratory syndrome coronavirus 2 (SARS-CoV-2), is the causative agent of the
2019 coronavirus disease (COVID-19) (1). The COVID-19 virus was first reported
in December 2019 in Wuhan, China, and the World Health Organization (WHO)
declared the outbreak of the COVID-19 virus an international concern on January
30, 2020, and on March 11, 2020, it was declared a global pandemic (2-4).
According to the National Center for Immunization and Respiratory Diseases,
high-risk groups for severe illness from COVID-19 include People aged 65 and
over, immunocompromised people, and people with chronic diseases such as
obesity (5). Obese people are at greater risk of severe COVID-19 (6). Studies
have shown that even obesity is a risk factor for severe disease in young
patients (7). As an urgent measure to limit the spread of the disease, many
governments around the world imposed quarantines, forcing millions of people to
stay at home and maintain isolation for extended periods (8), although these
measures led to the control of the interruption of the transmission chain,
these conditions had an unprecedented impact on the lives of the general
public, including forced inactivity along with changes in people's eating
habits, which are often associated with emotional problems and stress (9-11).
During the quarantine period, the consumption of unhealthy food, the frequency
of snacks, and the frequency of main meals have increased, and it has also
caused people to lose control over eating (12). On the other hand, staying at home
during quarantine causes psychological distress, mood disorders, and sleep
disorders (13-16), which in turn may negatively affect eating behaviors
(17-20). In addition, reducing leisure activities, boredom, increasing the time
of watching TV and easy access to food can increase the number of snacks and
overeating (21, 22). All the mentioned factors provide the hypothesis of body
weight gain during the quarantine period, which may have metabolic consequences
shortly and also increase the risk of cardiovascular disorders.
Obesity
and related diseases are one of the most important public health problems in
developed and developing countries due to their impact on quality of life, life
expectancy, and financial healthcare issues, which can be caused by a large
number of biological, psychological, and social factors (23-25). Over the past
30 years, the prevalence of obesity has been steadily increasing, and bariatric
surgery is the most effective and durable option for this chronic medical
disease and its related diseases (26, 27). Several studies confirm bariatric
surgery due to a significant reduction in weight as well as a significant
reduction or improvement of various obesity-related diseases (28, 29). However,
there is considerable variability in long-term weight loss results (30), and
weight gain after surgery is a common concern (31). Weight gain after bariatric
surgery is more common in patients with depression, anxiety, low social
support, and unhealthy eating habits, such as increased snacking and loss of
control while eating (32-34). Evidence suggests that the COVID-19 virus
pandemic has negatively impacted eating behaviors, psychological distress, and
weight outcomes in bariatric surgery patients (35, 36). On the other hand, a
lot of concern about weight, anxiety, less weight loss, and weight regain were
shown in patients undergoing bariatric surgery during the COVID-19 virus
pandemic (36). Weight regain, in turn, can increase
the risk of severe COVID-19 infection, lead to the return of obesity-related
diseases, and reduce the quality of life of patients (31,37).
Although
many studies have been conducted regarding the prevalence of weight gain in the
general population during the coronavirus pandemic, there are few studies on
the effect of the coronavirus pandemic on the weight outcomes of patients after
bariatric surgery. Since these patients are more vulnerable to stressful
factors and their weight outcomes can have a significant impact on the
incidence of obesity-related diseases and reduce the quality of life, this
review study was conducted to help to know more and more precisely the
consequences of the coronavirus pandemic on the weight outcomes of patients
after bariatric surgery.
Materials and Methods
In this systematic review, a Prisma tool was used. The
question considered in this study is: How has Coronavirus affected the weight outcomes
of patients after bariatric surgery?
Search strategy
In the present study, researchers reviewed articles
published in Google Scholar, Science Direct, and Scopus databases since the
beginning of the Coronavirus pandemic (2019) until now (June 21, 2023). It should be noted that the findings based on book chapters and
conference abstracts were among the limitations. The authors also reviewed the
reference list of eligible articles. Selected keywords in the search strategy
included "Coronavirus" and "Weight outcomes" and
"Bariatric surgery".
Data were collected in EndNote X20 software and duplicate
studies were eliminated. The title and abstract of all obtained articles were
screened and irrelevant articles were removed. The full text of the remaining
articles was included in the study to find relevant studies that fit our
inclusion criteria. It should be noted that data extraction was done by two
researchers separately.
Inclusion and exclusion criteria
Criteria
for inclusion of studies included publication of articles in reputable
scientific databases, English language, access to the full text of articles,
and relevance to the research topic. Editorials, notes, reviews, and letters to
the editor were excluded.
Results
This
review study yielded seventeen studies on patients with previous bariatric
surgery (Table 1). The process of searching for articles and selecting them is
shown in Figure 1. In the initial search, a total of 153 articles from three
databases were found, and after removing 18 duplicates in EndNote X20 software,
135 articles remained and articles by title were reviewed and 27 articles
remained in the end. By reviewing the titles and abstracts of the remaining
articles, 17 articles were entered.
Table
1.
Studies on patients with a previous bariatric surgery.
|
Authors Name |
|
Year Of Study |
Country of Research |
Type of Study |
Title of the study |
Findings |
|
|
1 |
Haghighat et al. (50) |
|
2023 |
Iran |
Retrospective,
single-center study |
Impact
of the COVID-19 Pandemic on the Success of Bariatric Surgeries in Patients
with Severe Obesity |
The effectiveness of bariatric
surgery for weight loss decreased during the quarantine period caused by the
coronavirus. In this study, to evaluate the weight outcomes of patients after
bariatric surgery, the patients were divided into two groups. The first group
was patients who had bariatric surgery during the coronavirus pandemic and
were under quarantine due to the coronavirus pandemic. And the second group
was patients who had undergone bariatric surgery before the coronavirus
pandemic and were not affected by the quarantine. Weight loss and the
decrease in body mass index 1 year after the surgery, as well as excess
weight loss and total weight loss, were significantly higher in the second
group than in the first group. |
|
2 |
Salituro et al. (43) |
|
2023 |
Italy |
The
observational retrospective cohort study |
The
impact of psychological distress on weight regain in
post-bariatric patients during the COVID-19 pandemic: A latent profile
analysis |
43%
and 34% of the post-bariatric patients reported clinically significant
anxiety and depressive symptoms, respectively. 60% of patients reported
clinically significant disturbed sleep. Post-bariatric patients in the high
psychological distressed group regained a mean of 1.4 kg, while patients in
the low psychological distressed group lost a mean of 1.1 kg. This study showed a significant relationship between
psychological distress and weight regain in patients after bariatric surgery
during the COVID-19 quarantine. |
|
3 |
Antoinette Hu et al. (47) |
|
2021 |
USA |
Cross-sectional
study |
Associations
of COVID-19 Lockdowns on Eating Behaviors and Body Mass Index in Patients
with a History of Bariatric Surgery: a
Cross-Sectional Analysis |
71.43% of patients experienced
weight recurrence with an average increase in body mass index (BMI) of 2.83
kg/m2 during the quarantine due to COVID-19. Also, 15.24% of patients after bariatric surgery
qualified for loss of control while eating, which was significantly related
to emotional overeating. The results of this research showed that the
significant social adversities experienced during the COVID-19 pandemic have
a negative effect on the eating behaviors of patients after bariatric
surgery. |
|
4 |
Carolina Ferreira
Nicoletti et al. (48) |
|
2021 |
Brazil
|
Observational Study |
Nutritional inadequacies among post-bariatric patients
during COVID-19 quarantine in Sao Paulo, Brazil
|
Screening
of dietary habits and food intake of patients with a history of bariatric
surgery through three non-consecutive 24-h food recalls showed that many
patients failed to receive the recommended daily protein and the
recommendation for frequent animal protein intake during social isolation.
Furthermore, about a quarter of these patients’ diets consisted of
ultra-processed foods. |
|
5 |
Conceição et al. (36) |
|
2021 |
Portugal |
longitudinal study |
Eating behaviors and
weight outcomes in post-bariatric surgery patients during the COVID-19
pandemic: A three-year longitudinal study |
COVID-19 lockdown resulted in
higher weight concern, grazing behavior, and negative urgency that increase
the risk of weight regain among post-bariatric patients. |
|
6 |
Athanasiadis
et al. (40) |
|
2021 |
USA |
case-control
study |
How
are bariatric patients coping during the coronavirus disease 2019 (COVID-19)
pandemic? Analysis of factors known to cause weight regain among
postoperative bariatric patients |
The
patient’s mental health condition was deteriorating during social isolation.
Nearly half of the patients reported increases in their depression (44.2%),
nervousness (54.7%), snacking (62.6%), loss of control when eating (48.2%),
and decreases in healthy food eating (45.5%), and activity (55.2%), all of
which led to weight regain. Weight regain was more
prevalent among patients after 18 months of surgery and they regained more
than 2 kg during an average of 47 days of COVID-19 lockdown. 43.6% of
patients gained weight after surgery. |
|
7 |
Durão et al.(42) |
|
2021 |
Portugal |
cross-sectional
study |
Confinement
During the COVID-19 Pandemic After Metabolic and Bariatric
Surgery—Associations Between Emotional Distress, Energy-Dense Foods, and Body
Mass Index |
Among postoperative bariatric
patients, higher reported levels of emotional distress during the COVID-19
lockdown
are associated with increased EDF consumption. Sweets
consumption was a subcategory of EDF significantly positively associated with
the odds of a worse outcome in BMI change. |
|
8 |
Messiah
et al. (44) |
|
2021 |
USA |
Retrospective
chart review |
Substance
Use, Mental Health, and Weight-Related Behaviors During the COVID-19 Pandemic
Among Metabolic and Bariatric Surgery Patients |
Post-bariatric
patients who completed their postoperative period during quarantine
experienced more sleep problems, anxiety, and substance use than other
patients who followed up before social isolation. The depression rate was
high in both groups. |
|
9 |
El Moussaoui et al. (60) |
|
2021 |
Belgium |
case-control
study |
Impact
of COVID-19 Lockdown on Short-Term Results After Laparoscopic Sleeve
Gastrectomy |
The purpose of this study was to
compare the percentage of total weight loss (%TWL), and excess weight loss
(%EWL) of patients in the first postoperative year between patients who
underwent primary bariatric surgery between June 2019 and October 2019 (1-year
postoperative period affected by COVID-19 lockdown; COV-group), and a control
group operated between June 2018 and October 2018 (1-year postoperative
period not affected by COVID-19 lockdown; CONTROL-group). The mean TWL and
EWL were lower in first-group patients compared to second-group patients at
one year from bariatric surgery. |
|
10 |
Sisto et al. (35) |
|
2020 |
Italy |
case-control
study |
The
psychological impact of COVID-19 pandemic on patients included in a bariatric
surgery program |
The
coronavirus pandemic led to increased psychological distress in patients with
a current or past history of obesity, reducing the quality of life and
affecting dietary compliance. Analysis of post-bariatric patients showed a
relationship between snacking, hunger, eating impulsivity, and anxiety,
stress, and/or depression symptoms. |
|
11 |
Andreu et al. (41) |
|
2020 |
Spain |
cross-sectional
exploratory |
Patients
Undergoing Bariatric Surgery: a Special Risk Group
for Lifestyle, Emotional and Behavioral Adaptations During the COVID-19
Lockdown. Lessons from the First Wave |
Dietary habits were affected in
72% of the participants, with 83.5% reporting having more sedentary
behaviors; 27% and 36% showing depression and anxiety, respectively; and 45%
of participants reporting bad sleep quality. Regarding changes in the use of any
substance, the use increased in the majority of patients who were previously
users. Self-perception of one’s health and fears related to COVID-19 were
only moderate. Finally, emotional eating and time since bariatric surgery
were statistically significant risk factors for predicting weight gain |
|
12 |
de
Luis et al. (38) |
|
2020 |
Spain |
Cross-sectional
study |
Factors
Related to Weight Gain in Subjects with Sleeve Gastrectomy During Lockdown by
the COVID-19 Pandemic |
An
increase in self-reported body weight among the patients during the interview
was associated with a decrease in physical activity and the loss of
face-to-face visits to the nutrition unit. 64% of patients became overweight after surgery. The increase in self-reported
body weight was 3.8±2.1 kg during the 7 weeks of confinement. |
|
13 |
Félix et al. (45) |
|
2020 |
Portugal |
Cross-sectional
study |
A
preliminary study on the psychosocial impact of COVID-19 lockdown in
post-bariatric surgery women: the importance of eating behavior, health care
access, and social support |
58.3% of post-bariatric patients
reported perceived weight gain during the COVID-19 lockdown. Also, 54.1% of
patients reported limited access to social support and 50% limited access to
medical care. |
|
14 |
Jimenez
et al. (54) |
|
2020 |
Spain |
Cross-sectional
study |
Psychosocial,
Lifestyle, and Body Weight Impact of COVID-19-Related Lockdown in a Sample of
Participants with Current or Past History of Obesity in Spain |
Changes in mood, negative changes in eating
habits, consumption of unhealthy foods, and weight gain were among the
adverse effects of the coronavirus pandemic on patients who underwent
bariatric surgery. |
|
15 |
Murtha et al. (39) |
|
2020 |
USA |
Cross-sectional
study |
Impact
of COVID-19 on the Postoperative Bariatric Surgery Patient Experience |
COVID-19 affected the
postoperative bariatric surgery patient experience via 3 mechanisms: (1) it
disrupted dietary and physical activity routines due to facility closures and
fear of COVID-19 exposure; (2) it required patients to transition their
follow-up care to telemedicine delivery; and (3) it increased stress due to
financial and psychosocial challenges. |
|
16 |
Vitiello et al. (49) |
|
2019
- 2020 |
Italy |
Retrospective
study |
Impact
of COVID-19 Lockdown on Short-term Weight Loss in a Single Italian
Institution |
Two
groups of patients were evaluated. The first group of patients underwent
bariatric surgery before the start of the coronavirus pandemic (year 2019) and the second group of patients underwent bariatric
surgery during the virus pandemic (year 2020). Weight loss at 1, 3,
and 6 postoperative months in the 2019 group was significantly higher at any
point of follow-up when compared to 2020. Social restrictions and
non-attendance at clinical appointments were among the factors affecting the
weight outcomes of patients after surgery, because in 2019, no patient missed
clinical appointments in the first 6 months, while in 2020, the rate of
nonattendance at 1, 3, and 6 months was 15.6%, 18.7%, and 31.3%. |
|
17 |
de Angulo et al. (65) |
|
2019 – 2020 |
Spain |
Case–control study |
Influence of the lockdown due to COVID-19 on weight-loss results
during the first year after sleeve gastrectomy |
Population lockdown by COVID-19
did not get worse short-term results of bariatric surgery. |
Figure 1. Flow diagram of the study selection for the review process.
The
effects of the coronavirus pandemic and subsequent quarantine on post-bariatric
surgery patients are shown in Figure 2.
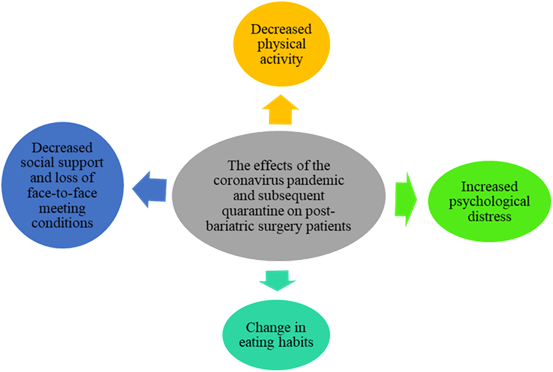
Figure 2. The effects of the coronavirus
pandemic on post-bariatric surgery patients.
Physical activity conditions among post-bariatric surgery patients
during the quarantine:
Social quarantine has reduced physical activity in patients with a
history of bariatric surgery (38, 39). In the study of Athanasiadis et al.,
55.2% of patients with bariatric surgery, reported decreased physical activity,
which plays an important role in weight regain in the postoperative period
(40). Andreu et al. showed that 83.5% of patients with bariatric surgery during
the coronavirus pandemic, reported more sedentary behaviors than before (41).
Mental health conditions among post-bariatric surgery patients
during the quarantine:
Among post-bariatric surgery patients, higher reported levels of
emotional distress during the COVID-19 quarantine (42). In the study by
Athanasiadis et al., out of 208 patients with bariatric surgery, 54.7% reported
nervousness, 44.2% depression, and 36.2% loneliness (40). Salituro et al.
showed that 43% and 34% of the post-bariatric patients reported clinically
significant anxiety and depressive symptoms, respectively. In this study, 60%
of patients reported clinically significant disturbed sleep (43). According to
Andreu et al., out of 156 patients with bariatric surgery, 27% reported
depression, 36% anxiety, and 45% bad sleep quality (41). Messiah et al.'s study
showed that post-bariatric patients who completed their postoperative period
during quarantine experienced more sleep problems, anxiety, and substance use
than other patients who followed up before social isolation (44).
Finally, Mandatory quarantine caused by the coronavirus has created
many psychological challenges for patients with bariatric surgery, which
increases the risk of weight regain and this issue highlights the importance of
regular follow-up (36, 39, 43, 45, 46).
Food habits among post-bariatric surgery patients during the
quarantine:
Andreu et al. showed that dietary habits were affected in 72% of
patients with bariatric surgery during social quarantine (41). Patients with
previous bariatric surgery, experienced an increase in snacking (35, 40), loss
of control while eating (40, 45, 47), consumption of unhealthy foods (38, 40),
and grazing behavior (36) during social quarantine. On the other hand,
emotional eating and time since bariatric surgery were statistically
significant risk factors for predicting weight gain (41). Moreover, Nicoletti
et al. stated that many patients failed to receive the recommended daily
protein and the recommendation for frequent animal protein intake during social
isolation, and the intake of highly processed foods had increased (48).
Social support conditions among post-bariatric surgery patients
during the quarantine:
Social restrictions and non-attendance at clinical appointments
were among the factors affecting the weight outcomes of patients after
bariatric surgery during the COVID-19 quarantine (39, 49). In the study of de
Luis et al., an increase in self-reported body weight among the post-bariatric
surgery patients during the interview was associated with a decrease in loss of
face-to-face visits during the COVID-19 quarantine (38). According to Félix et
al., 54.1% of patients reported limited access to social support and 50%
limited access to medical care (45).
Weight gain among post-bariatric surgery patients during the
quarantine:
COVID-19 quarantine increases the risk of weight regain among
post-bariatric patients (36, 43, 50). According to Athanasiadis et al., 43.6%
of patients gained weight after bariatric surgery. In this study, weight regain
was more prevalent among patients after 18 months of surgery and they regained
more than 2 kg during an average of 47 days of COVID-19 quarantine (40). In the
study of de Luis et al., 64% of patients became overweight after surgery. The
increase in self-reported body weight was 3.8±2.1 kg during the 7 weeks of
quarantine (38). Félix et al. showed that 58.3% of post-bariatric patients
reported perceived weight gain during the COVID-19 quarantine (45). Also, in
Antoinette Hu et al.'s study, 71.43% of patients experienced weight recurrence
with an average increase in body mass index (BMI) of 2.83 kg/m2 during the
COVID-19 quarantine (47).
Discussion
One of the high-risk groups for severe illness caused by the
coronavirus is people with chronic diseases, including obesity (5). Bariatric
surgery and subsequent weight loss significantly reduce the risk of serious
consequences caused by the coronavirus (51). Weight loss is more evident in the
first year after surgery because it increases the individual's motivation and
creates healthy life habits in many patients (52). Among the measures that were
taken to control the chain of transmission of the coronavirus pandemic in many
governments, was to establish quarantine and force people to stay at home and
maintain isolation for a long time (8), these conditions had an unprecedented
negative impact on the lives of the general public (9-11). Patients who have undergone
bariatric surgery are no exception to this rule. Both pre
and post-operative management of post-bariatric patients requires a
multidisciplinary approach, including nutrition and dietary interventions,
physical activity as well as psychological support focused on promoting
adherence to treatment and the adoption of healthy lifestyles over the short
and longer term (58). During post-operative follow-ups, bariatric patients
often feel a sense of isolation, abandonment, and ambivalence toward surgery outcomes
(59) which could negatively affect the quality of life, psychological distress,
and eating habits (10). Social distancing and the great stress burden generated
by the COVID-19 pandemic might enhance those feelings, increasing psychological
distress, undermining healthy lifestyle compliance, and fostering weight regain
and comorbidities recurrence in at-risk post-bariatric patients (60). As we
observed in the review of studies, several psychosocial and physical factors
can cause weight gain for patients with a history of bariatric surgery during
the coronavirus pandemic. In this study, we categorized factors affected by the
pandemic era into four categories: physical activity, mental health, food
habits, and social support.
Decreased physical activity
The studies extracted in the current research showed that one of
the negative factors affecting the coronavirus pandemic and the subsequent
quarantine and social isolation of patients who have undergone bariatric
surgery is the reduction of physical activity. In the research of Athanasiadis
et al., 55.2% of people who had bariatric surgery reported a decrease in
physical activity during the coronavirus pandemic and the resulting quarantine,
and the results of this study showed that reducing physical activity is one of
the risk factors for gaining weight after bariatric surgery during the
coronavirus pandemic (40). Also, in the study of De Luis et al., it was shown
that during the coronavirus pandemic, more than half of the patients became
overweight after bariatric surgery, and this weight gain is associated with a
decrease in physical activity (38). The amount of exercise performed per week
by the patients overall decreased (53). Mandated closures of gymnasiums likely
contributed to decreases in exercise in some patients. Planning and counseling
by specialists to increase physical activity after bariatric surgery is an
important factor in creating favorable outcomes of surgery.
Increased psychological distress
Another negative factor affecting the coronavirus pandemic and the
subsequent quarantine and social isolation of the mentioned patients is an
increase in psychological distress in patients who have undergone bariatric
surgery. The results of Conceição et al.'s study showed that the increase in
anxiety in patients undergoing bariatric surgery was one of the negative
effects of the coronavirus pandemic on patients (36). Jimenez et al also stated
in their study that one of the adverse effects of the coronavirus pandemic on
patients who underwent bariatric surgery was mood changes (54). Also reported
an increase in depression, loneliness, and anger as the adverse effects of the
coronavirus pandemic on patients who underwent bariatric surgery (40). The
mentioned factors, in turn, can negatively affect the eating behaviors of
patients (17-20), and provide the hypothesis of body weight gain after surgery.
Sisto et al.'s study showed that there was a significant relationship between
symptoms of anxiety, depression, and stress and increased snack consumption,
desire to eat, and hunger in patients after bariatric surgery during the
coronavirus pandemic (35). According to Salituro et al., there is a significant
relationship between psychological distress and weight regain in patients after
bariatric surgery during the COVID-19 quarantine (43). Mental health problems
can last longer than the infection itself and spread more widely than the
pandemic (55). Targeted psychological support during times of increased stress,
anxiety, depression, and mood changes is essential for fragile people such as
patients after bariatric surgery. For these reasons, it has been recommended
that mental health professionals should be on the “front line” (56). Even
telephone-only contact can be experienced as helpful by patients who have had
bariatric surgery (57) and can be effective in the treatment of anxiety and
depression (58).In only one study, the rate of
depression was not affected by the quarantine and was high in both groups of
patients before and after social isolation, and this may be due to different
perceptions of patients (44).
Change in eating habits
The coronavirus pandemic and the quarantine of people caused an
increase in the consumption of unhealthy food, the frequency of snacking and
overeating, as well as the loss of control over eating (12). Nicoletti et al.'s
study showed that almost 90% of patients after bariatric surgery did not
receive the necessary protein during the coronavirus pandemic, and 25% of them
consumed too much processed foods (59). Jimenez et al also considered the
consumption of unhealthy foods as one of the adverse effects of the coronavirus
pandemic on patients after bariatric surgery (54). The results of Athanasiadis
et al.'s study showed that the risk factors for weight gain among
post-bariatric surgery patients during the coronavirus quarantine include
decreased consumption of healthy food, increased consumption of snacks,
overeating, and loss of control while eating (40). During the quarantine,
patients further out of their surgery date were eating relatively healthier
food (40), which may be explained by greater experience with dietary adherence
(53). In addition, patients in the first days of quarantine were eating
unhealthier food, which might be due to the initial high stress that social
distancing inflicted on patients (40). To solve the mentioned problems,
specialists can provide online guidance to their patients through mobile phone
programs and encourage patients to have healthy eating habits, consume healthy
foods, and do appropriate sports activities. For patients with limited access
to the Internet, direct phone calls can still be a valuable source of
encouragement (40). In this regard, a recent study showed that about half of
post-bariatric surgery patients did not attend face-to-face nutrition
counseling sessions during the quarantine, and this was a risk factor for their
weight regain (38).
Decreased social support and loss of face-to-face meeting
conditions
One of the risk factors for gaining weight after bariatric surgery
during the coronavirus pandemic and the subsequent quarantine and social
isolation reducing the presence of patients in clinical appointments for
post-surgery consultation and replacing face-to-face consultations with
telephone consultations (49, 60). De Luis et al.'s study showed that the loss
of face-to-face meetings with a nutrition consultant is one of the factors
influencing the weight gain of patients after bariatric surgery (38). Also,
Vitiello et al. stated in their study that the rate of weight loss after
bariatric surgery in patients who underwent surgery during the coronavirus
pandemic was significantly lower than in patients who underwent surgery before
the start of the pandemic, which is the reason was social restrictions and not
attending clinical appointments. In this study, the rate of nonattendance of
post-bariatric surgery patients during the coronavirus pandemic in clinical
appointments at the first 1, 3, and 6 months after surgery was 15.6%, 18.7%,
and 31.3%. (49). These findings warn doctors about the need to closely monitor
these patients and the importance of facilitating access to consultations and
promoting social support. With clinics reducing availability and even closing
during a pandemic, alternative means of providing support to patients are
needed. Social media platforms can at least partially fill this gap, but the
feasibility and effectiveness of this form of support are only recently been
researched (61). Telehealth visits have been well received by patients. For
example, physical training via telehealth is helpful for patients preparing for
bariatric surgery (62). There is strong evidence for the acceptability,
effectiveness, and cost savings of tele behavioral health interventions in
general (63) and in the bariatric population more specifically (64).
Weight gain after bariatric surgery
The results obtained from the review of studies show the negative
impact of the coronavirus pandemic and the subsequent quarantine and social
isolation on the weight outcomes of patients after bariatric surgery. The rate
of weight loss after surgery is significantly lower in patients who underwent
bariatric surgery during the coronavirus pandemic and were quarantined compared
to patients who underwent surgery before the virus pandemic (36, 49, 60). On
the other hand, some studies showed that patients who underwent bariatric
surgery during the coronavirus pandemic gained weight after the surgery. In
Andreu et al.'s study, 72% of participants believed their weight had changed
during quarantine. Weight gain was the most frequent change reported (86%),
with a mean of 2.1 ± 2.8 kg (41). De Luis et al stated in their study that the
coronavirus pandemic causes weight gain in patients who have undergone
bariatric surgery, and during the coronavirus pandemic, 64.4% of patients
became overweight after bariatric surgery (38). Athanasiadis et al.'s study
also showed that 43.6% of patients who underwent bariatric surgery gained
weight during the coronavirus pandemic (40). The results of Félix et al.'s
study showed that 58.3% of people who underwent bariatric surgery gained weight
within 36 months after the surgery during the quarantine caused by the
coronavirus pandemic (45). The results of Jimenez et al.'s study also indicate
that one of the adverse effects of the coronavirus pandemic on patients who
underwent bariatric surgery is weight gain after surgery (54). While most
studies have shown the negative impact of the coronavirus pandemic on the
weight outcomes of the aforementioned patients, the results of the research by
De Angulo et al showed that the coronavirus pandemic did not worsen the weight
outcomes of patients after bariatric surgery (65). Regular follow-up of
post-bariatric surgery patients with a team of psychologists in addition to
physicians and nutritionists can help them to achieve self-management and
reduce the burden on the health system in the long term.
Conclusions
The coronavirus pandemic and the
subsequent quarantine and social isolation have affected many areas of the
lives of people who have undergone bariatric surgery, which has ultimately
caused a negative impact on the results of weight outcomes of patients after
surgery. Post-bariatric surgery patients during the coronavirus pandemic were
mentally and physically prone to quarantine complications, and many of these
patients reported weight gain during this period. These findings will
contribute to developing effective therapeutic strategies to address
difficulties faced by post-bariatric surgery patients, which can be further
exacerbated under circumstances such as this challenging pandemic. Therefore,
specialized care and interventions are needed to address behaviors that lead to
weight regain during future pandemics or in the post-coronavirus era in
vulnerable patients after bariatric surgery, as the weight regained in these
patients is difficult to lose afterward.
Author contribution
SHM and SH wrote and completed the manuscript. SHM
designed wrote and edited the manuscript comprehensively. SHM and SH
confirmed the final version of the paper.
Conflict of interest
The authors declare that they have no conflicts of interest.
Acknowledgments
This article is a systematic review study that does not have a code
of ethics. This article is a study without human or animal samples. There were
no ethical considerations in this study.
References
1. Pedrosa C, Goto-Silva L, Temerozo JR,
Souza LRQ, Vitória G, Ornelas IM, et al. Non-permissive SARS-CoV-2 infection in
human neurospheres. Stem Cell Res. 2021;54:102436.
2. Organization WH. WHO timeline-Covid-19. 2020. URL: https://www who int/news-room/detail/08-04-2020-who-timeline---covid-19.
2020.
3. Rothan HA, Byrareddy SN. The
epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak.
Journal of autoimmunity. 2020;109:102433.
4. Sohrabi C, Alsafi Z, O'neill N, Khan
M, Kerwan A, Al-Jabir A, et al. World Health Organization declares global
emergency: A review of the 2019 novel coronavirus (COVID-19). International
journal of surgery. 2020;76:71-6.
5. Muscogiuri G, Pugliese G, Barrea L,
Savastano S, Colao A. Commentary: obesity: the “Achilles heel” for COVID-19?
Metabolism-Clinical and Experimental. 2020;108:154251.
6. Stefan N, Birkenfeld AL, Schulze MB, Ludwig DS. Obesity and
impaired metabolic health in patients with COVID-19. Nature Reviews
Endocrinology. 2020;16(7):341-2.
7. Kass DA, Duggal P, Cingolani O. Obesity could shift severe
COVID-19 disease to younger ages. The Lancet. 2020;395(10236):1544-5.
8. Wang Y, Wang Y, Chen Y, Qin Q. Unique epidemiological and
clinical features of the emerging 2019 novel coronavirus pneumonia (COVID‐19)
implicate special control measures. Journal of medical virology.
2020;92(6):568-76.
9. Di Renzo L, Gualtieri P, Pivari F, Soldati L, Attinà A, Cinelli G, et al. Eating habits and lifestyle
changes during COVID-19 lockdown: an Italian survey. Journal of translational
medicine. 2020;18:1-15.
10. Zouhal H, Ben Abderrahman A, Khodamoradi A, Saeidi A, Jayavel A, Hackney AC, et al.
Effects of physical training on anthropometrics, physical and physiological
capacities in individuals with obesity: A systematic review. Obesity reviews.
2020;21(9):e13039.
11. Salgin B, Norris SA, Prentice P, Pettifor JM, Richter LM, Ong KK, et al. Even transient
rapid infant weight gain is associated with higher BMI in young adults and
earlier menarche. International journal of obesity. 2015;39(6):939-44.
12. Ammar A, Brach M, Trabelsi K, Chtourou
H, Boukhris O, Masmoudi L, et al. Effects of COVID-19
home confinement on eating behavior and physical activity: results of the
ECLB-COVID19 international online survey. Nutrients. 2020;12(6):1583.
13. Cellini N, Canale N, Mioni G, Costa S. Changes in sleep
pattern, sense of time and digital media use during COVID‐19 lockdown in Italy.
Journal of sleep research. 2020;29(4):13074.
14. Mazza C, Ricci E, Biondi S, Colasanti M, Ferracuti
S, Napoli C, et al. A nationwide survey of psychological distress among Italian
people during the COVID-19 pandemic: immediate psychological responses and
associated factors. International journal of environmental research and public
health. 2020;17(9):3165.
15. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate
psychological responses and associated factors during the initial stage of the
2019 coronavirus disease (COVID-19) epidemic among the general population in
China. International journal of environmental research and public health.
2020;17(5):1729.
16. Wolf MS, Serper M, Opsasnick L, O'Conor RM, Curtis L, Benavente JY, et al.
Awareness, attitudes, and actions related to COVID-19 among adults with chronic
conditions at the onset of the US outbreak: a cross-sectional survey. Annals of
internal medicine. 2020;173(2):100-9.
17. Cardi V, Leppanen J, Treasure J. The effects of negative and
positive mood induction on eating behavior: A meta-analysis of laboratory
studies in the healthy population and eating and weight disorders. Neuroscience
& Biobehavioral Reviews. 2015;57:299-309.
18. Gluck ME. Stress response and binge eating disorder. Appetite.
2006;46(1):26-30.
19. Roberts CJ, Campbell IC, Troop N. Increases in weight during
chronic stress are partially associated with a switch in food choice towards
increased carbohydrate and saturated fat intake. European Eating Disorders
Review. 2014;22(1):77-82.
20. Hawkley LC, Thisted RA, Cacioppo JT. Loneliness predicts
reduced physical activity: cross-sectional & longitudinal analyses. Health
Psychology. 2009;28(3):354-63.
21. Francis HM, Stevenson RJ, Oaten MJ, Mahmut MK, Yeomans MR. The
immediate and delayed effects of TV: impacts of gender and processed-food
intake history. Frontiers in psychology. 2017;8:1616.
22. Moynihan AB, Van Tilburg WA, Igou ER, Wisman A, Donnelly AE,
Mulcaire JB. Eaten up by boredom: consuming food to escape awareness of the
bored self. Frontiers in psychology. 2015;6:369.
23. van der Valk ES, van den Akker EL, Savas M, Kleinendorst
L, Visser JA, Van Haelst MM, et al. A comprehensive
diagnostic approach to detect underlying causes of obesity in adults. Obesity
reviews. 2019;20(6):795-804.
24. Sinha I, Mondal N, Sen J. Effects of socio-economic,
demographic and lifestyle variables on overweight and obesity among rural
Rajbanshi post-menopausal women of India. Anthropologischer
Anzeiger; Bericht uber die biologisch-anthropologische
Literatur. 2018;75(3):251-62.
25. Arroyo-Johnson C, Mincey KD. Obesity epidemiology trends by
race/ethnicity, gender, and education: National Health Interview Survey,
1997–2012. Gastroenterology Clinics of North America. 2016;45(4):571.
26. O’Brien PE, Hindle A, Brennan L, Skinner S, Burton P, Smith A,
et al. Long-term outcomes after bariatric surgery: a systematic review and
meta-analysis of weight loss at 10 or more years for all bariatric procedures
and a single-center review of 20-year outcomes after adjustable gastric
banding. Obesity surgery. 2019;29(1):3-14.
27. Sjöström L. Review of the key results from the Swedish Obese
Subjects (SOS) trial–a prospective controlled intervention study of bariatric
surgery. Journal of internal medicine. 2013;273(3):219-34.
28. El Moussaoui I, Van Vyve E, Johanet H, Dabrowski A, Piquard A, Delaunay T, et al.
Laparoscopic sleeve gastrectomy for morbid obesity in a Belgian-French
prospective multicenter study: outcomes and predictors weight loss failure.
Acta Chirurgica Belgica. 2021;121(6):413-19.
29. Ahn SM. Current issues in bariatric surgery for adolescents
with severe obesity: durability, complications, and timing of intervention.
Journal of obesity & metabolic syndrome. 2020;29(1):4-11.
30. Courcoulas AP, King WC, Belle SH,
Berk P, Flum DR, Garcia L, et al. Seven-year weight trajectories and health
outcomes in the Longitudinal Assessment of Bariatric Surgery (LABS) study. JAMA
surgery. 2018;153(5):427-34.
31. Karmali S, Brar B, Shi X, Sharma AM, de Gara C, Birch DW.
Weight recidivism post-bariatric surgery: a systematic review. Obesity surgery.
2013;23(11):1922-33.
32. Devlin MJ, King WC, Kalarchian MA,
Hinerman A, Marcus MD, Yanovski SZ, et al. Eating
pathology and associations with long‐term changes in weight and quality of life
in the longitudinal assessment of bariatric surgery study. International
Journal of Eating Disorders. 2018;51(12):1322-30.
33. Conceição EM, Fernandes M, de Lourdes M, Pinto-Bastos A, Vaz
AR, Ramalho S. Perceived social support before and after bariatric surgery:
association with depression, problematic eating behaviors, and weight outcomes.
Eating and Weight Disorders-Studies on Anorexia, Bulimia, and Obesity.
2020;25(3):679-92.
34. Conceição E, Mitchell JE, Vaz AR, Bastos AP, Ramalho S, Silva
C, et al. The presence of maladaptive eating behaviors after bariatric surgery
in a cross-sectional study: the importance of picking or nibbling on weight
regain. Eating behaviors. 2014;15(4):558-62.
35. Sisto A, Vicinanza F, Tuccinardi D, Watanabe M, Gallo IF,
D’Alessio R, et al. The psychological impact of COVID-19 pandemic on patients
included in a bariatric surgery program. Eating and Weight Disorders-Studies on
Anorexia, Bulimia, and Obesity. 2020;26:1-11.
36. Conceição E, de Lourdes M, Ramalho S, Félix S, Pinto-Bastos A,
Vaz AR. Eating behaviors and weight outcomes in bariatric surgery patients
amidst COVID-19. Surgery for Obesity and Related Diseases. 2021;17(6):1165-74.
37. Sarwer DB, Steffen KJ. Quality of
Life, Body Image and Sexual Functioning in Bariatric Surgery Patients. Eur Eat Disord Rev.
2015;23(6):504-8.
38. de Luis D, Izaola O, Primo D, Gómez
E, Torres B, Gómez JJL, et al. Factors related to weight gain in subjects with
sleeve gastrectomy during lockdown by the COVID-19 Pandemic. Obesity Surgery.
2021;31(5):2197-202.
39. Murtha JA, Alagoz E, Breuer CR, Eierman L, Jawara D,
Farrar-Edwards D, et al. Impact of COVID-19 on the Postoperative Bariatric
Surgery Patient Experience. Annals of Surgery. 2023;277(4):745-51.
40. Athanasiadis DI, Hernandez E, Hilgendorf W, Roper A, Embry M,
Selzer D, et al. How are bariatric patients coping during the coronavirus
disease 2019 (COVID-19) pandemic? Analysis of factors known to cause weight
regain among postoperative bariatric patients. Surgery for Obesity and Related
Diseases. 2021;17(4):756-64.
41. Andreu A, Flores L, Molero J, Mestre C, Obach
A, Torres F, et al. Patients undergoing bariatric surgery: a special risk group
for lifestyle, emotional and behavioral adaptations during the COVID-19
lockdown. Lessons from the first wave. Obesity Surgery. 2022;32:441-9.
42. Durão C, Vaz C, de Oliveira VN, Calhau
C. Confinement during the COVID-19 pandemic after metabolic and bariatric
surgery—associations between emotional distress, energy-dense foods, and body
mass index. Obesity Surgery. 2021;31(10):4452-60.
43. Salituro N, Landi G, Garelli S, Balsamo F, Rottoli
M, Cattivelli R, et al. The impact of psychological
distress on weight regain in post-bariatric patients
during the COVID-19 pandemic: A latent profile analysis. Journal of
Psychosomatic Research. 2023;165:111144.
44. Messiah SE, Uppuluri M, Xie L, Schellinger JN, Mathew MS, Ofori
A, et al. Substance use, mental health, and weight-related behaviors during the
COVID-19 pandemic among metabolic and bariatric surgery patients. Obesity
surgery. 2021;31:3738-48.
45. Félix S, de Lourdes M, Ribeiro I, Cunha B, Ramalho S, Vaz AR,
et al. A preliminary study on the psychosocial impact of COVID-19 lockdown in
post-bariatric surgery women: the importance of eating behavior, health care
access, and social support. Current Psychology. 2021;40(12):6275-81.
46. Jimenez A, de Hollanda A, Palou E,
Ortega E, Andreu A, Molero J, et al. Psychosocial, lifestyle, and body weight
impact of COVID-19-related lockdown in a sample of participants with current or
past history of obesity in Spain. Obesity surgery. 2021;31:2115-24.
47. Hu A, Harvey A, Rogers AM, Rigby A, Butt M. Associations of
COVID-19 Lockdowns on Eating Behaviors and Body Mass Index in Patients with a
History of Bariatric Surgery: a Cross-Sectional
Analysis. Obesity Surgery. 2023;33(4):1099-107.
48. Nicoletti CF, Esteves GP, Genario R,
Santo MA, de Cleva R, Gualano B, et al. Nutritional inadequacies among
post-bariatric patients during COVID-19 quarantine in Sao Paulo, Brazil.
Obesity Surgery. 2021;31:2330-4.
49. Vitiello A, Berardi G, Velotti N,
Schiavone V, Musella M. Impact of COVID-19 Lockdown on Short-term Weight Loss
in a Single Italian Institution. Obesity Surgery. 2021;31(7):3365-8.
50. Heinberg LJ, Steffen K. Social Isolation and Loneliness During
the COVID-19 Pandemic: Impact on Weight. Current Obesity Reports.
2021;10(3):365-70.
51. Uccelli M, Cesana GC, De Carli SM, Ciccarese
F, Oldani A, Zanoni AAG, et al. COVID-19 and obesity: is bariatric surgery
protective? Retrospective analysis on 2145 patients undergone
bariatric-metabolic surgery from high volume center in Italy (Lombardy).
Obesity surgery. 2021;31(3):942-8.
52. Tettero OM, Aronson T, Wolf RJ, Nuijten MA, Hopman MT, Janssen IM. Increase in physical
activity after bariatric surgery demonstrates improvement in weight loss and
cardiorespiratory fitness. Obesity surgery. 2018;28(12):3950-7.
53. Bergh I, Kvalem IL, Risstad H, Sniehotta FF.
Preoperative predictors of adherence to dietary and physical activity
recommendations and weight loss one year after surgery. Surgery for Obesity and
Related Diseases. 2016;12(4):910-8.
54. Jimenez A, de Hollanda A, Palou E,
Ortega E, Andreu A, Molero J, et al. Psychosocial, lifestyle, and body weight
impact of COVID-19-Related lockdown in a sample of participants with current or
past history of obesity in Spain. Obesity surgery. 2021;31(5):2115-24.
55. Reardon S. Ebola's mental-health wounds linger in Africa:
healthcare workers struggle to help people who have been traumatized by the
epidemic. Nature. 2015;519(7541):13-5.
56. Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and
COVID-19: mental health burden and strategies. SciELO
Brasil. 2020;42:232-5.
57. Voils CI, Adler R, Strawbridge E, Grubber J, Allen KD, Olsen
MK, et al. Early-phase study of a telephone-based intervention to reduce weight
regain among bariatric surgery patients. Health Psychology. 2020;39(5):391.
58. Lamb T, Pachana NA, Dissanayaka N.
Update of recent literature on remotely delivered psychotherapy interventions
for anxiety and depression. Telemedicine and e-Health. 2019;25(8):671-7.
59. Nicoletti CF, Esteves GP, Genario R,
Santo MA, de Cleva R, Gualano B, et al. Nutritional inadequacies among
post-bariatric patients during COVID-19 quarantine in Sao Paulo, Brazil.
Obesity Surgery. 2021;31(5):2330-4.
60. El Moussaoui I, Navez J, El Moussaoui K, Barea-Fernandez M, Schaeken A, Closset J. Impact of
COVID-19 Lockdown on Short-Term Results After Laparoscopic Sleeve Gastrectomy.
Obesity Surgery. 2021;31(6):2614-8.
61. Koball AM, Jester DJ, Domoff SE, Kallies KJ, Grothe KB, Kothari SN. Examination
of bariatric surgery Facebook support groups: a content analysis. Surgery for
Obesity and Related Diseases. 2017;13(8):1369-75.
62. Baillot A, Boissy P, Tousignant M,
Langlois M-F. Feasibility and effect of in-home physical exercise training
delivered via telehealth before bariatric surgery. Journal of telemedicine and
telecare. 2017;23(5):529-35.
63. Bashshur RL, Shannon GW, Bashshur N, Yellowlees PM. The
empirical evidence for telemedicine interventions in mental disorders.
Telemedicine and e-Health. 2016;22(2):87-113.
64. Bradley LE, Thomas JG, Hood MM, Corsica JA, Kelly MC, Sarwer DB. Remote assessments and behavioral interventions
in post-bariatric surgery patients. Surgery for Obesity and Related Diseases.
2018;14(10):1632-44.
65. de Angulo DR, Román AB, Ruiz VM, Vázquez PJG, Merino GR,
Escandell MÁO, et al. Influence of the lockdown due to COVID-19 on weight-loss
results during the first year after sleeve gastrectomy. Cirugía
Española (English Edition). 2021;99(6):428-32