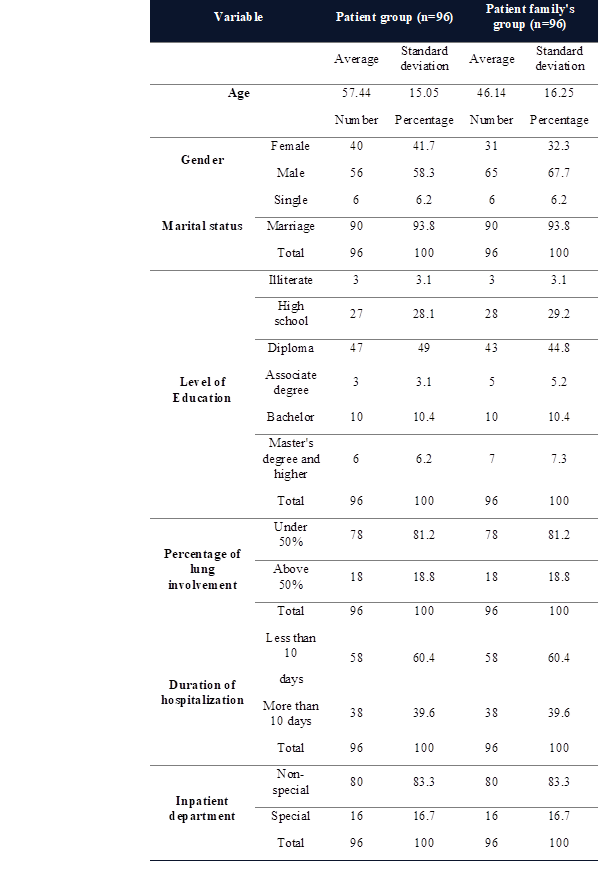
Table 1. Demographic characteristics and COVID-19 disease in study
participants.
Prevalence and
factors related to post-traumatic stress disorder (PTSD) in patients with
COVID-19 and their families admitted to 22 Bahman Hospital in Neyshabur
Mehdi Bakaeian 1, Zeinab Jalambadani 2, Fatemeh Khorashadizadeh
3, Hadi Olyaei 4, Mahboobe Gholami 5,6*
1 Department of Nursing, Neyshabur
University of Medical Sciences, Neyshabur, Iran
2 Department of Public Health,
Faculty of Medical, Torbat jam, Iran
3 Department of Epidemiology and
Biostatistics, Neyshabur University of Medical Sciences, Neyshabur, Iran
4 22 Bahman Hospital, Neyshabur
University of Medical Sciences, Neyshabur, Iran
5 Noncommunicable Diseases Research
Center, Neyshabur University of Medical Sciences, Neyshabur, Iran
6 Department of Midwifery, Neyshabur
University of Medical Sciences, Neyshabur, Iran
*Corresponding
Author: Mahboobe Gholami
* Email: gholamim26279@gmail.com
Abstract
Diseases such as COVID-19 can be associated with the development of
mental disorders such as PTSD in patients or their families, which can last for
years. Therefore, this study investigated the prevalence and factors associated
with post-traumatic stress disorder (PTSD) in patients with COVID-19 and their
families admitted to 22 Bahman Hospital in Neyshabur in 2020. In this
descriptive cross-sectional study, 96 patients and 96 family members in
Neyshabur were included using available and voluntary sampling. PTSD in
individuals was assessed by completing the DSM-5(PCL-5) checklist and
interviewing. Demographic information including gender, age, level of education
and marital status was also collected. Information related to COVID-19 disease
including the patient's pulmonary involvement, duration of hospitalization and
ward was recorded. In both groups, the majority of participants were men (56%),
married people (90%), and people with a diploma (49%). The mean score of PTSD in the patient group and the patient family group was
35.5 and 33.5, respectively. All subjects in the patient group and the patient
group had PTST disorder (PTSD score>18). In the group of patients with COVID-19,
the severity of post-traumatic stress disorder was severe in 14.6%, moderate in
21.9%, and mild in the rest. Also, the incidence of PTSD among patients'
families was 16.7% severe, 31.2% moderate and the rest mild. Regression
analysis showed that the variables of hospitalization and duration of
hospitalization could predict stress disorder in patients at 53.9% and 24.2%.
Given the widespread coronavirus in communities as well as the prevalence of
PTSD in patients and their families, control measures should be considered to
improve the mental health of these individuals.
Keywords: Coronavirus, COVID-19, PTSD, Trauma
Introduction
Post-traumatic
stress disorder (PTSD) is the most common and important mental disorder that
occurs in a situation where a person experiences a lot of stress with fear of
death of themselves or others (1). Certain types of events such as
natural disasters such as floods and earthquakes, the spread of infectious
diseases as well as physical or sexual abuse are significantly associated with
the spread of PTSD (2-5). The
prevalence of PTSD is affected by the severity, duration and proximity of the
accident (3). Previous studies have shown that
PTSD is the most common psychological problem after an epidemic due to
traumatic conditions (4). Outbreaks appear to be exacerbated
during pregnancy and in patients with dementia (6). Even family members of patients
with COVID-19 are experiencing increased stress. Poor knowledge of the
structure, behavior, and mechanisms of virus transmission, uncertainty overtime
to control the disease, quarantine of patients and families, and death of
family members have led to widespread fear and anxiety and loss of confidence
in individuals. On the other hand, patients with coronation and their families
experience difficult and stressful conditions due to hearing bad news from
those around them and the media, the heavy burden of treatment costs and other
related factors. The World Health Organization (WHO) estimates that 30 to 50
percent of the population in areas affected by the SARS-CoV-2 coronavirus
epidemic suffer from various psychological problems, especially PTSD. At the
same time, it has been reported that people with PTSD are more at risk of
suicidal ideation, suicide attempt and suicide-related death (5). This is so important that even
physicians are advised to include PTSD as part of a common history when taking
histories of patients with coronavirus (7, 8). Patients with COVID-19, especially
in the severe form of the disease, are usually admitted to infectious wards in
isolation. These patients may experience loneliness, anger, anxiety,
depression, insomnia, and post-stress symptoms due to perceived social
isolation, dangerous conditions, uncertainty about the future, physical
discomfort, drug side effects, and fear of transmitting the virus to others.
Experience the accident. These effects can negatively affect the social,
occupational and quality of life of these people in the short and long term (9). Patients connected to ventilators
are restless and confused about what is happening. Therefore, it is predictable
that many people who are discharged from intensive care unit survivors after
treatment will experience depression, anxiety, post-traumatic stress disorder,
and other mental health problems. A UK study reported that more than 50 percent
of patients admitted to the intensive care unit showed severe signs of anxiety,
depression and post-traumatic stress disorder after discharge (10). In this regard, the prevalence of
symptoms and diagnostic criteria for PTSD during the coronavirus epidemic in
Italy has been reported up to 49.7% (11). The prevalence of PTSD at the time
of the previous epidemic of coronavirus strains was reported to be about 32% (12). Naturally, in such a situation,
the mental condition of the family and those around the patients is also
unfavorable. In a study in Japan of more than 16,000 participants, including
family and friends of patients with COVID 19, the results showed that most of
them were fearful and anxious. In this study, PTSD scores in women under 60
were more than was reported from other individuals and age groups (13). The families of patients with
COVID-19 have also been identified as a trauma group so that the monitoring of
their mental state and, if necessary, counseling measures should be considered
for them (14). Otherwise, in the near future we
are likely to see an increase in the incidence of PTSD in the whole community (15). PTSD can be very common even long
after the initial exposure to trauma. If proper and timely action is not taken
for counseling and psychotherapy, this disorder will challenge people for many
years to come. Therefore, in the current situation where patients with COVID-19
and their families are under a lot of stress, it seems necessary to study the
prevalence of this disorder among patients and their family members to plan
counseling and treatment measures. So far, several studies have been conducted
on the prevalence of PTSD among COVID-19 survivors worldwide, but studies to
examine the psychological consequences of COVID-19 disease among patients and
their companions in developing areas such as Iran are limited (16). Given that socio-cultural
differences, as well as demographic characteristics, affect the prevalence and
severity of PTSD in individuals, conducting such a study is a priority. This
study aimed to investigate the prevalence and factors associated with
post-traumatic stress disorder (PTSD) in patients with COVID 19 and their
families admitted to 22 Bahman Hospital in Neyshabur in 2020.
Materials and Methods
Study
design and selection of participants
The
present study was a descriptive cross-sectional study conducted in 2020. The
study consisted of 19 patients with COVID 19 admitted to 22 Bahman Hospital in
Neyshabur and their family members. Sampling was non-random and available and
voluntary. In this way, the purpose of the study and the method of work
(completing the questionnaire and checklist) was explained to patients and
their families. If these individuals met the inclusion criteria and also
expressed their consent to participate, a written consent form would be
obtained from them. Finally, 96 patients and 96 family members were included in
the study. This study aimed to determine the prevalence of PTSD in patients
with COVID-19 and their families in Neyshabur and to determine the factors
associated with this disorder. Inclusion criteria for patients included:
hospitalization based on COVID-19 diagnosis, and ability to answer questions
(stability of disease condition). Exclusion criteria for patients included:
outpatients with a maximum hospital stay of one day and a history of
psychiatric medication use at least one month before admission to
hospitalization. Criteria for inclusion of patients' family members in the
study were; Be a first-degree relative of the patient who wants to participate
in the research and is willing to cooperate at the time of the patient's
discharge. Exclusion criteria for a family member should also include relatives
of the patient whose patient does not meet the inclusion criteria. Ethical
criteria in the research, including ensuring the confidentiality of
information, sufficient and necessary explanation of the working method and
guidance in referring to counseling centers depending on the severity of the
disorder were observed. This research is based on a research design with ethics
code IR.NUMS.REC.1399.035.
Data
collection
Based
on the coordination with the hospital, an arrangement was made to inform the
research team one day before the possible discharge of COVID 19 patient, so
that one of the research colleagues would be present at the patient's discharge
and complete the checklist to diagnose the disorder along with the interview.
Data were collected by completing a demographic information questionnaire as
well as a DSM-5 (PCL-5) checklist and interview. When completing the checklist
and interviewing, the research colleague met with them and their families in
full compliance with hygiene principles and at the time of discharge.
Demographic information included gender, age, level of education, and marital
status. Also, information related to COVID-19 disease including the patient's
pulmonary involvement, duration of hospitalization and ward were recorded.
DSM-5
(PCL-5) checklist
The
post-traumatic stress disorder checklist was designed based on the DSM-5
(PCL-5). This checklist was prepared by Withers, Leitz,
Kane, Palmeier, Marx, and Ashnor
(1993), based on the criteria of the Fifth Edition Diagnostic and Statistical
Manual of Mental Disorders, for the US National Center for Post-Traumatic
Stress Disorder as a diagnostic aid. This checklist contains 17 five-choice
items. Of these 17 items, 5 were related to the signs and symptoms of re-experiencing
a traumatic event, 7 were related to the signs and symptoms of emotional
numbness and avoidance, and 5 were related to the symptoms and symptoms. The
scoring method is in the form of Likert from one to five and the total score of
the articles (85-17) is considered as the individual score (17). A score of 35 is considered as the
cut-off point in most studies (18-20). The validity
and reliability of this tool have been reviewed and confirmed in previous
studies (17-22). In the
present study, Cronbach's alpha coefficient for the whole scale was 0.90.
Depending on the scores obtained from the stress checklist after injury and
according to the range of scores, individuals were divided into three groups.
Thus, individuals with scores ranging from 18-28, 29-56 and 57-85 were divided
into mild, moderate and severe PTSD groups, respectively. A score of 17 meant
that there was no evidence of this disorder.
Statistical
analysis
The
number and relative frequency of participants were calculated and reported
based on various parameters. Spearman correlation analysis was also used to
determine the correlation between individuals' PTSD scores and demographic
variables and COVID-19 disease. Linear regression analysis was used to evaluate
the effect of demographic variables and COVID-19 disease on the severity of
PTSD. Data were analyzed by SPSS v.16 software at a significance level of 0.05.
Results
Data
analysis was performed on 192 patients (96 patients and 96 families of these
patients). Demographic characteristics, length of hospital stay, ward, and
percentage of lung involvement in patients and families of patients with COVID
19 are listed in Table 1. In both groups, the majority of participants were men
(56%), married people (90%), and people with a diploma (49%). The percentage of
lung involvement in most of the subjects (78%) was less than 50% who were
hospitalized for less than 10 days (58%) in non-specialized wards (80%).
Table 1. Demographic characteristics and COVID-19 disease in study
participants.
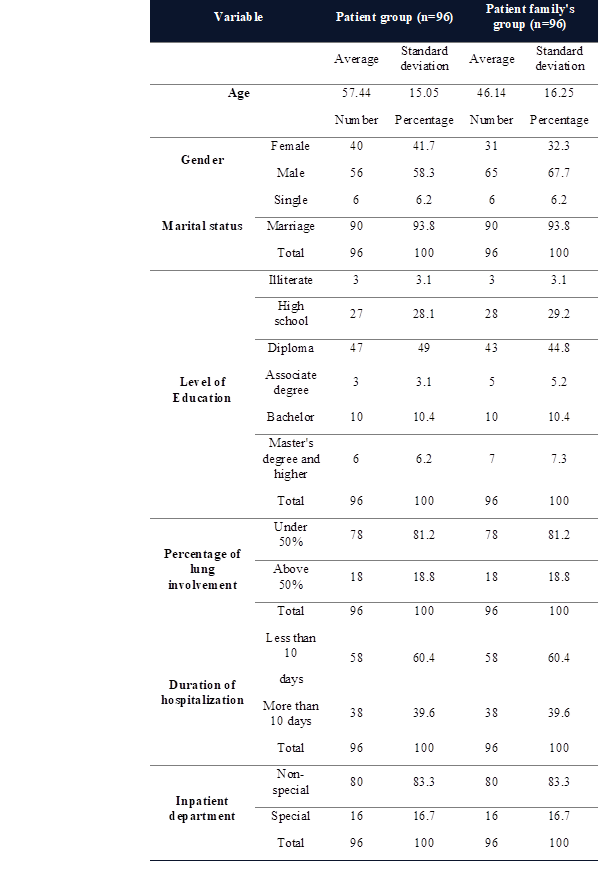
The
amount and severity of post-traumatic stress disorder (PTSD) in patients and
families of patients with COVID 19 were assessed using a questionnaire and the
results are listed in Table 2. The mean score of PTSD
in the patient group and the patient family group was 35.5 and 33.5,
respectively. This indicates that, on average, the severity of PTSD in patients
was slightly higher than in patients' families. All subjects in the patient
group and the patient group had PTSD, meaning that in this study, there was no
individual without this disorder among the participants. In the group of
patients with COVID-19, the severity of post-traumatic stress disorder was
severe in 14.6%, moderate in 21.9% and mild in the rest. The percentage was
severe, 31.2% was moderate and the rest was mild.
Table 2. Number and percentage of
participants based on the extent and severity of PTSD.
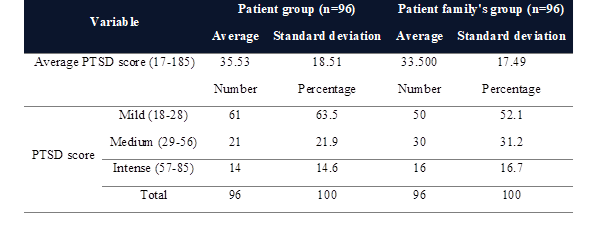
The
correlation between PTSD scores in patients and their families with demographic
characteristics and disease parameters were examined by the Spearman
correlation test and the results are presented in Table 3. According to the
results of Table 3, a significant positive correlation was observed between the
variables of involvement percentage, type of hospitalization and duration of
hospitalization with the severity of post-traumatic stress disorder in both
groups.
The
longer the hospital stay and the percentage of lung involvement, the higher the
stress disorder score was reported. Also, those admitted to the intensive care
unit reported higher stress scores. Compared to the patient group, a higher
correlation was found between the severity of PTSD and the percentage of
pulmonary involvement and inpatient ward among patients' families. If the
duration of hospitalization was more correlated with the severity of PTSD among
patients. Also, no significant correlation was found between stress disorder and
demographic variables such as gender, age, level of education and marital
status.
Table 3. Correlation of PTSD scores with demographic variables and
parameters of COVID-19 disease in patient groups and patients' families.
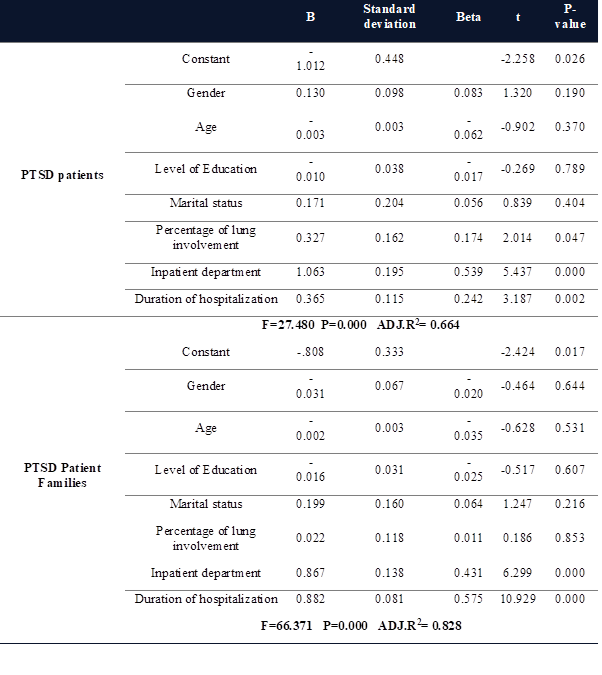
The
results of regression analysis to evaluate the effect of demographic variables
and parameters of COVID-19 disease on the severity of PTSD are presented in
Table 4. In both groups, none of the demographic variables, including age,
gender, education, and marital status, affected the severity of PTSD. The
results of the regression test showed that the variables of hospitalization,
length of hospitalization and percentage of lung involvement of patients can
predict stress disorder in the families of patients with 43.1%, 57.5% and
1.10%, respectively. These results mean that family members of patients who
have been hospitalized in the intensive care unit for more than 10 days, and
their lung involvement rate is more than 50%; Higher levels of stress disorder
have also been reported. Also, the results of data analysis by regression test
in the patient group showed that only the variables of hospitalization and
duration of hospitalization (and not the percentage of lung involvement) can predict
stress disorder, at 53.9% and 24.2%. These results indicate that patients who
have been hospitalized in the intensive care unit for more than 10 days have
also reported a higher rate of stress disorder (Table 4).
Table 4. The effect of demographic variables and parameters of COVID-19
disease on the severity of PTSD in patient groups and patients' families.
Discussion
In this study, the severity of PTSD in patients with COVID-19 and
their families in 2020 was evaluated. The effect of some demographic variables
as well as parameters related to COVID-19 on the severity of PTSD was also
analyzed. According to the results, post-traumatic stress disorder had a
significant correlation with the percentage of lung involvement, type of ward
and length of hospital stay. In patients, the variables of hospitalization and
duration of hospitalization had a significant effect on the severity of PTSD.
Also, three variables of lung involvement percentage, type of hospitalization
ward and length of hospitalization in the families of patients with COVID were
able to significantly predict stress disorder. The present study showed that
14.6% of patients and 16.7% of their families had a severe type of this
disorder and the rest of the participants suffered from moderate and mild
types. A previous meta-analysis study found that during previous coronavirus
epidemics, the prevalence of PTSD was about 32% (12). In the case of SARS-CoV-2, a study
in Italy found that the prevalence of PTSD symptoms among COVID-19 survivors
was about 30% (23). However, the results of another
study in Italy showed that PTSD was diagnosed in 10.4% of the subjects. The
results of this study are more consistent with the present study. In a
case-control study, PTSD scores in the case group were significantly higher
than in the control group (16, 23). In general,
the difference in the prevalence of PTSD among COVID-19 patients can be due to
various reasons, including cultural-religious differences, as well as the
distance between the test and the completion of COVID-19 disease. Because it
has been shown that with increasing duration after discharge, patients' PTSD
scores increase by 20% (23). In the present study, contrary to
the studies mentioned, the DSM-5 (PCL-5) checklist was completed on the day of
discharge. In general, previous studies show that approximately 5 to 10 percent
of men and 10 to 12 percent of women will experience the disorder in their
lifetime. The lifetime prevalence of this disorder in the general population
has been reported to be about 8%. About 5-15% of other people may also have
subclinical forms of the disorder (3). The present study showed that PTSD
is higher in patients admitted to the intensive care unit and their families
who feel the risk of death closer. Previous studies have also shown that
post-traumatic stress disorder is more common, especially in people who feel
that death is imminent or imminent for any reason. For example, in a study of
16,000 participants in Japan, people who had COVID-19 in one of their family
members showed more psychological distress than others (13). Following the outbreak of SARS in
2003, both health care workers and quarantined individuals showed signs of
post-traumatic stress disorder. PTSD was also reported to be the most common
long-term psychiatric disorder among them. The incidence of this disorder in
two years after the outbreak of SARS was 47.8% (4). Risk factors for increasing the
severity of PTSD symptoms include female gender, living in a city with the
disease, poor sleep quality, and experience with a dangerous physical illness,
but there is a significant relationship between PTSD and age and education. In
another study, in groups under 60 years of age, respondents who had a patient
with COVID-19 had a higher score of psychological stress, regardless of gender,
and this difference was statistically significant (13). Another study reported that female
gender, poor economic status, and fear could predict the severity of PTSD in
patients with coronary heart disease (24). In the present study, patients
admitted to intensive care units and their companions showed a higher severity
of PTSD, which could be due to fear of death. In general, some differences in
the findings between the current study and some previous studies may be due to
cultural-religious differences. Another reason may depend on the timing of the
study. While the present study was performed approximately 2 years after
coronary heart disease, some other studies were performed only a few months
after the onset of the disease (11).
This
suggests that stress levels and mental health problems can probably be reduced
over time and familiarity with the risks and how to deal with the disease.
Previous studies have also reported that the symptoms of PTSD are moderately
high in nurses and physicians and all people working in hospital wards and are
higher in women working in these wards (9). Although the disorder is more
common in women under normal circumstances (other than coronary heart disease),
its prevalence in women can be attributed to the more stressful roles they have
to play at home during quarantine, as well as the quarantine effect at home.
Staying attributed (25). The prevalence of PTSD, depression
and sleep disorders increases during quarantine. Fear of getting sick is the
most important factor of psychological distress and living in a completely
limited environment is very effective on the duration of sleep and mental
health (26). In another study, PTSD and
depression and anxiety were more common in medical staff who were directly
associated with patients (25). Although exposure rates, work
experience, occupational support and social support, quarantine, age, gender
and marital status have been reported to be associated with PTSD (27). In the present study age, gender
and status Marriage had nothing to do with PTSD. The reason for this difference
could be the difference in the statistical population, because, in the study,
participants included the treatment staff of the statistical community and in
the present study, the participants were patients admitted to their families.
The results of the present study proved that PTSD is a common
disorder among patients and families involved with COVID-19. This disorder can
severely affect the quality of life of the person and those around them so that
the person is involved with its complications for years after the end of
COVID-19. At present, it seems that in addition to efforts at various levels to
prevent the spread of coronary heart disease and other worrying conditions,
special attention should be paid to mental health issues. Programs offered for
screening for psychiatric disorders, including anxiety and depression,
especially PTSD among patients and their families, and case management by
employing psychiatrists, psychologists, and other related medical groups,
especially in quarantine cases due to the severity of vulnerabilities and it
seems necessary to create peace and trust in the people (8).
This
study has strengths and limitations that should be noted. This study is one of
the few studies that has been performed on the effect of COVID-19 on the
incidence of PTSD in patients and their relatives in the world. Also in this
study, the modification effect of several parameters such as gender, education,
marital status, length of hospital stay, percentage of pulmonary involvement
and hospitalization on PTSD severity were measured. However, the present study
has some limitations as well. First, due to the physical and psychological
effects of COVID-19, patients' energy and motivation to respond were low.
Second, patients' families sometimes had time constraints to respond due to the
patient's haste to discharge. Also, the physical distance was observed when
communicating with patients and their families, which can affect effective
communication with them.
Conclusions
In this study, the rate of PTSD in
patients with COVID-19 and their families was assessed by a valid
questionnaire. The effect of individual factors and parameters related to
COVID-19 on the severity of PTSD was also investigated. The results showed that
all subjects in the patient group and the patient family group showed mild to
severe degrees of PTSD. On average, the severity of PTSD in patients was
slightly higher than in the patients' families. The effect of none of the
parameters of gender, age, education and marital status on the incidence of
PTSD was significant. However, in the group of patients, the variables of
hospitalization and duration of hospitalization had a significant effect on the
severity of PTSD. The results of this study indicate that COVID-19 disease and
exposure to the resulting fear and anxiety cause PTSD in both patients and
their families. Given the widespread of coronavirus in communities and the
prevalence of PTSD in patients and their families, control measures should be
considered to improve mental health for these individuals. These measures may
include screening for psychiatric disorders such as anxiety and depression,
especially PTSD among patients and their families, and managing PTSD cases by
employing psychiatrists, psychologists, and other medical groups.
Author contribution
MGh managed the manuscript, study design, controlling the project and
fulfilled the data processing and compiled some sections of the article. MB,
ZJ, FKh and HO were involved in
some sections of the manuscript like collected data, data processing and
performed statistical analyses. MGh wrote the
whole manuscript. All authors revised the article comprehensively and confirmed
the final edited version of the paper.
Conflict of interest
The authors reported no potential conflict of interest.
Acknowledgments
Hereby, the Vice Chancellor
for Research of Neyshabur School of Medical Sciences due to the approval and
support of this project. And I appreciate the management and treatment staff of
22 Bahman Hospital in Neyshabur, patients with COVID-19 and their families for
their cooperation.
References
1. Salmanian
M, Salehi M, Hooshyari Z. Global prevalence of posttraumatic stress disorder
(PTSD) during and after coronavirus pandemic: A study protocol for a systematic
review and meta-analysis. Iran J Psychiatry. 2020;15(3):252.
2. Association AP. Diagnostic and
Statistical Manual of Mental Disorders.[Y Seyed Mohammadi, Persian Trans.].
Tehran: Ravan Publisher. 2013.
3. Kilpatrick DG, Resnick HS,
Milanak ME, Miller MW, Keyes KM, Friedman MJ. National estimates of exposure to
traumatic events and PTSD prevalence using DSM‐IV and DSM‐5 criteria. J Trauma Stress. 2013;26(5):537-47.
4. Mak IWC, Chu CM, Pan PC, Yiu
MGC, Chan VL. Long-term psychiatric morbidities among SARS survivors. Gen Hosp
Psychiatry. 2009;31(4):318-26.
5. Dutheil F, Mondillon L, Navel
V. PTSD as the second tsunami of the SARS-Cov-2 pandemic. Psychol Med.
2021;51(10):1773-4.
6. Wan S-H. Life and Death, Hope
and Despair in the Era of Coronavirus Disease 2019. JAMA cardiology.
2020;5(9):985-.
7. Rehman S, IFTEKHAR A, ABDULLAH
M. History of Infection Outbreaks and Mental Health Issues: Awareness for
Corona-virus Neuropsychiatric Coverage.
8. Zhang J, Wu W, Zhao X, Zhang
W. Recommended psychological crisis intervention response to the 2019 novel
coronavirus pneumonia outbreak in China: a model of West China Hospital. Precis
Clin Med. 2020;3(1):3-8.
9. Tang W, Hu T, Hu B, Jin C,
Wang G, Xie C, et al. Prevalence and correlates of PTSD and depressive symptoms
one month after the outbreak of the COVID-19 epidemic in a sample of
home-quarantined Chinese university students. J Affect Disord. 2020;274:1-7.
10. Jubran A, Lawm G, Duffner LA,
Collins EG, Lanuza DM, Hoffman LA, et al. Post-traumatic stress disorder after
weaning from prolonged mechanical ventilation. Intensive Care Med.
2010;36(12):2030-7.
11. Forte G, Favieri F, Tambelli R,
Casagrande M. COVID-19 pandemic in the Italian population: validation of a
post-traumatic stress disorder questionnaire and prevalence of PTSD
symptomatology. Int J Environ Res Public Health. 2020;17(11):4151.
12. Rogers JP, Chesney E, Oliver D,
Pollak TA, McGuire P, Fusar-Poli P, et al. Psychiatric and neuropsychiatric presentations
associated with severe coronavirus infections: a systematic review and
meta-analysis with comparison to the COVID-19 pandemic. The Lancet Psychiatry.
2020;7(7):611-27.
13. Tanoue Y, Nomura S, Yoneoka D,
Kawashima T, Eguchi A, Shi S, et al. Mental health of family, friends, and
co-workers of COVID-19 patients in Japan. Psychiatry Res. 2020;291:113067.
14. Sekowski M, Gambin M, Hansen K,
Holas P, Hyniewska S, Wyszomirska J, et al. Risk of Developing Post-traumatic
Stress Disorder in Severe COVID-19 Survivors, Their Families and Frontline
Healthcare Workers: What Should Mental Health Specialists Prepare For? Front
Psychiatry. 2021;12.
15. Chang MC, Park D, editors.
Incidence of post-traumatic stress disorder after coronavirus disease.
Healthcare; 2020: Multidisciplinary Digital Publishing Institute.
16. Tarsitani L, Vassalini P,
Koukopoulos A, Borrazzo C, Alessi F, Di Nicolantonio C, et al. Post-traumatic
stress disorder among COVID-19 survivors at 3-month follow-up after hospital
discharge. J Gen Intern Med. 2021;36(6):1702-7.
17. Weathers FW, Litz BT, Herman
DS, Huska JA, Keane TM, editors. The PTSD Checklist (PCL): Reliability,
validity, and diagnostic utility. annual convention of the international
society for traumatic stress studies, San Antonio, TX; 1993: San Antonio, TX.
18. Blanchard EB, Jones-Alexander
J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist
(PCL). Behav Res Ther. 1996;34(8):669-73.
19. Ruggiero KJ, Ben KD, Scotti JR,
Rabalais AE. Psychometric properties of the PTSD Checklist—Civilian version. J
Trauma Stress. 2003;16(5):495-502.
20. Kharamin SA, GORJI R, GHOLAM
ZS, AMINI K. The prevalence rate of post-traumatic stress disorder (PTSD) in the
rape victims of Kohgiloyeh and Boyairahmad province during (2011-2012). 2012.
21. Blevins CA, Weathers FW, Davis
MT, Witte TK, Domino JL. The posttraumatic stress disorder checklist for DSM‐5
(PCL‐5): Development and initial psychometric evaluation. J Trauma Stress.
2015;28(6):489-98.
22. Goudarzi MA. Based on the
reliability and validity of the scale of post-traumatic stress. J Psychol.
2003;7(2).
23. Janiri D, Carfì A, Kotzalidis
GD, Bernabei R, Landi F, Sani G, et al. Posttraumatic stress disorder in patients
after severe COVID-19 infection. JAMA psychiatry. 2021;78(5):567-9.
24. Carmassi C, Foghi C, Dell'Oste
V, Cordone A, Bertelloni CA, Bui E, et al. PTSD symptoms in healthcare workers
facing the three coronavirus outbreaks: What can we expect after the COVID-19
pandemic. Psychiatry Res. 2020;292:113312.
25. Blekas A, Voitsidis P,
Athanasiadou M, Parlapani E, Chatzigeorgiou AF, Skoupra M, et al. COVID-19:
PTSD symptoms in Greek health care professionals. Psychological Trauma: Theory,
Research, Practice, and Policy. 2020;12(7):812.
26. Liu CH, Zhang E, Wong GTF, Hyun
S. Factors associated with depression, anxiety, and PTSD symptomatology during
the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry
Res. 2020;290:113172.
27. Johnson SU, Ebrahimi OV,
Hoffart A. PTSD symptoms among health workers and public service providers
during the COVID-19 outbreak. PloS one. 2020;15(10):e0241032.