P53 expression in
colorectal carcinomas study at a tertiary health care center in South Kerala
Alina Ajoy Thomas 1*, Meeta Thomas 1, Jessy
M.M 1
1 Department of Pathology, Pushpagiri
Institute of Medical Sciences & Research Centre, Thiruvalla, Kerala, India
Corresponding Authors: Alina Ajoy
Thomas
* Email: alina.ajoy@gmail.com
Abstract
Introduction: Colorectal carcinoma (CRC) ranks as the third most ubiquitous cancer
globally and the fourth primary source of cancer-related mortality. Loss of the
p53 gene is vital in the conversion of colorectal adenoma into carcinoma. The
study aims to evaluate the prevalence of p53 expression and investigate its
correlation with diverse clinicopathological parameters, providing valuable
insights into the dynamics of colorectal cancer in the specified region.
Methods: A total of 42 CRC cases from tertiary healthcare center in South
Kerala, India, were sampled between December 2018 and January 2021.
Comprehensive clinical data and clinicopathological parameters were collected,
followed by histomorphological and immunohistochemical evaluations. The results
were then correlated with clinicopathological variables.
Results: Patients aged 45 to 82 years (mean 63.5)
exhibited a predilection for the left colon (57%) and rectum (33%), with
symptoms ranging from abdominal pain to weight loss. Histologically, 95.2% were
adenocarcinomas, mostly moderately differentiated (57.1%). Tumor extension (T3:
57%) and lymph node involvement (N1: 29%) were prevalent, with Stage II tumors
(38.1%) most frequent. P53 immunoreactivity was observed in 83.3% of cases,
correlating with moderately differentiated grades, higher tumor extensions (T3/T4),
N1/N2 lymph node statuses, and Stage II/III tumors. No significant associations
were found with age, sex, lesion site, or tumor type. P53 nuclear positivity,
identified through IHC analysis, provides crucial insights into cancer biology,
prognosis, and potential therapeutic implications. The finding highlights
significant associations between p53 expression and key clinicopathological
parameters. P53 positivity is notably higher in moderately differentiated
tumors (Grade) and T3/T4 tumor extensions compared to well and poorly
differentiated grades and T1/T2 extensions, respectively. Significant links
were also observed with lymph node status (N1/N2 > N0) and tumor stage
(S2/S3 > S1), indicating a strong correlation between p53 expression and
advanced disease characteristics. However, no significant associations were
found with age, sex, lesion site, or tumor type. The novelty of our study lies
in the focused exploration of p53 expression in colorectal carcinomas. By
specifically investigating the correlation between p53 expression and various
clinicopathological parameters, we contribute a unique perspective to the
understanding of the molecular characteristics of colorectal cancer. This
targeted approach enhances the visibility of novel insights that our study
brings to the field of p53 expression in the context of colorectal carcinomas.
Conclusion: Our investigation
underscores that p53 overexpression is particularly prominent in advanced-stage
colorectal cancer cases and those having LNM, further supporting its role as an
adverse prognostic marker in this context.
Keywords: Colorectal carcinoma, P53, Immunohistochemistry, Lymph node, Prognosis
Introduction
Colorectal carcinoma (CRC), a prevalent malignancy
worldwide, poses a significant health challenge due to its high ubiquity and
associated morbidity and mortality In
2020, it resulted in approximately 1.9 million new cases and 930,000 deaths.
Factors such as age, family history, genetics, and lifestyle choices, including
diet, physical activity, smoking, and alcohol consumption, influence the risk
of developing CRC. Incidence and mortality rates vary significantly worldwide,
with Europe and Australia/New Zealand experiencing the highest rates and Africa
and Asia the lowest. Projections suggest a 63% increase in incidence and a 73%
rise in mortality by 2040 (1), driven by population growth, ageing, and
evolving risk factors. While CRC is
preventable and treatable, early detection and proper management are crucial,
emphasizing the importance of effective strategies for primary prevention,
screening, diagnosis, and treatment
Also, it is the third most ubiquitous cancer in men
along with the second most ubiquitous cancer in women across the globe.
However, in India, the incidence rates of colon cancer are notably lower in
comparison to other cancer types (2) In India, the annual incidence of CRC
stands at 4/100, 000, with Kerala reporting a slightly higher rate at 5.5/100,
000. In recent years, extensive research has focused on identifying specific
biomarkers and clinicopathological variables that can provide valuable insights
into the prognosis and management of CRC. One such key molecular player in the
context of colorectal cancer is the p53 protein a critical tumor suppressor
protein, which plays a fundamental role in preserving genomic stability along
with regulating cell cycle progression. Dysregulation of the p53 pathway, often
associated with p53 protein overexpression, has been involved in the
development along with progression of CRC (3).
CRC stands as a
complex malignancy characterized by a spectrum of clinical and pathological
features. Our study, encompassing various demographic and tumor-related factors
to unravel the intricacies of this disease. This investigation offered insights
into key aspects such as age distribution, gender variations, preferred
carcinoma sites, histological grading, tumor extension patterns, lymph node
involvement, and tumor staging (4). Additionally, our scrutiny extended to the
pivotal biomarker, p53, known for its association with cancer development and
prognosis. By comprehensively examining these demographic and tumor-related
factors, our study adds valuable insights to the intricate landscape of
colorectal adenocarcinoma. The focus on p53 expression further contributes to
the understanding of molecular markers with potential implications for
prognosis and targeted therapeutic interventions (Harris and Hollstein, 2013)
(5). The study aimed to determine the correlation between p53 expression and
clinicopathological parameters in CRC, focusing on tumor grade, extension,
lymph node status, and stage to elucidate the molecular implications for
prognosis and therapy.
Methods
This cross-sectional study involved CRC patients’
cases presented to the Department of Pathology at Pushpagiri Institute of
Medical Sciences and Research Centre, Thiruvalla, Kerala, India, between
December 2018 and January 2019. The study included a cohort of 42 patients for
analysis and relevant clinical data, encompassing variables such as age,
gender, colon subsite distribution, clinical presentation at diagnosis,
histopathological type, tumor grade, disease stage, and presence of LNM, were
collected from medical records for evaluation and correlation analysis.
Inclusion criteria encompassed all
histopathologically diagnosed cases of carcinoma in the colon and rectum,
comprising both biopsies and resected specimens.
Exclusion criteria
Comprised endoscopic
biopsies with corresponding resected specimens of the colon and resection
specimens from patients who underwent neoadjuvant chemotherapy.
Immunohistochemical (IHC) Staining for p53
IHC staining for the p53
protein was conducted using 5-micrometer sections acquired from formalin-fixed
paraffin-embedded blocks. These IHC-stained sections were evaluated alongside
H&E-stained specimens to determine the expression of p53 in CRC . The
interpretation of p53 immunostaining was based on whether it was positive or
negative. Also, positive staining was demarcated as the presence of nuclear
staining in ≥5% of cells per high-power field.
Data Analysis
The collected data was input into Microsoft Office
Excel 2019 spreadsheets and subsequently analysed using SPSS version 16.0
software. Associations between p53 expression and clinicopathological
parameters were assessed using Fisher’s exact test. A p-value less than 0.05
was deemed to be significant in statistical terms. The study findings were
presented in appropriate charts and tables.
Ethical Considerations
All procedures performed in
this study received approval from the Institutional Review Board (IRB) with
reference number 19666/2018, dated 17/01/2019. The research followed the
guidelines established in the Helsinki Declaration of 1964 along with its following
revisions. Written informed consent was not required, as determined by the IRB,
with a waiver granted for this purpose.
Results
The results demonstrate the patient population and the
characteristics of the colorectal adenocarcinoma cases under investigation. In
a cohort of 42 cases, we observed a diverse range of demographic and
tumor-related factors. As shown in Figure 1, the study group, patients’ ages spanned from
45 to 82 years, with the most substantial representation observed in the 61-70
years age category. The mean age at diagnosis was 63.5±10.60 years, and a
minority of patients, specifically 11.9% (n=5), were under the age of 50.

Figure 1. Age
Distribution within the study population.
Among the 42 cases examined
(as depicted in Figure 2), 19 were male, while 23 were female, resulting in a
male-to-female ratio of 0.8:1.

Figure 2. Gender wise
distribution among study population.
As illustrated in Figure 3, the observed tumor growth
exhibited a predilection for the colon and rectum’s left side, with 24 (57%)
cases occurring in this region, whereas 33 % cases were observed under rectum
site and 10 % were on left side Clinical presentations among these cases varied
and included symptoms such as abdominal pain, rectal bleeding, altered bowel
habits, signs indicative of intestinal obstruction, weight loss, and anaemia.
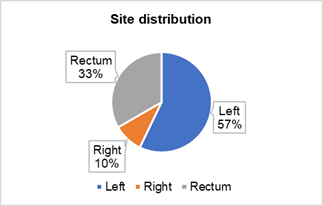
Figure 3. Distribution
of Carcinoma Sites within the Study Population.
As depicted in Figure 4, histological grading show vast majority of colorectal carcinomas,
accounting for 95.2% (n=40), were categorized as adenocarcinoma NOS. Within
this category, 57.1% (n=24) were moderately differentiated, 38.1% (n=16) were
well-differentiated, and a smaller proportion, 4.8% (n=2), were poorly differentiated.
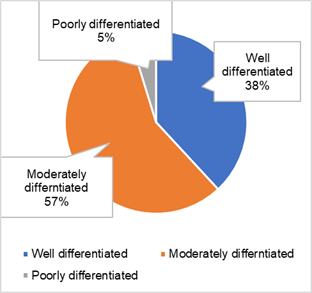
Figure 4. Histological
grading among study population.
This histology image (Figure 4.1) demonstrates that
moderately differentiated adenocarcinomas were predominantly observed in the
left colon within the study population.
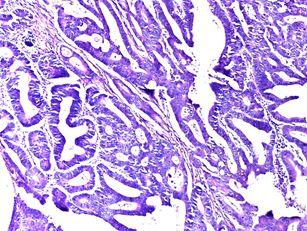
Figure 4.1. Moderately
differentiated adenocarcinoma – left colon (H&E).
As shown in
Figure 5 the remaining cases comprised two instances of mucinous carcinoma.
Among the tumors, 57% (n=24) exhibited infiltration extending beyond the
muscularis propria into the adjacent pericolic adipose tissue, designated as
T3, while 31% (n=13) were restricted to the muscularis propria, categorized as
T2 A smaller subset, 9.5% (n=4), showed infiltration into the visceral
peritoneum or adjacent organs, classified as pT4. Additionally, only one case
(2.4%) was identified as an early-stage T1 tumor.
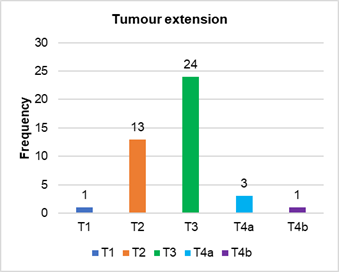
Figure 5. Distribution
of tumor extension among study population.
As indicated in Figure 6 in half of the cases, there
was no evidence of nodal involvement, whereas 29% were categorized as N1 and
21% as N2 were observed in study population.
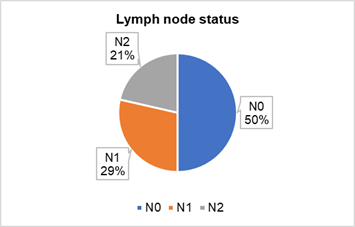
Figure 6. Distribution of
Lymph node status among study population.
As demonstrated in Figure 7, the most frequently
observed tumor stage was Stage II, with 38.1% (n=16) of cases, followed by
Stage I tumours at 33.3% (n=14), and Stage III at 28.6% (n=12).
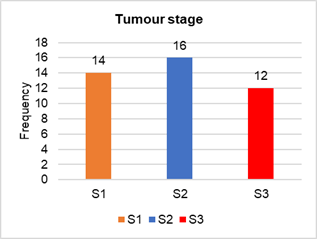
Figure 7. Distribution of
tumour staging among study population.
As depicted in Figure 8, p53 immunoreactivity
expression was detected in 35 cases of CRC, making up 83.3% of the study
cohort. Only seven cases (16.7%) displayed no p53 expression.
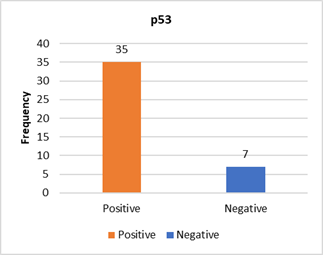
Figure 8. Expression of
p53 immunoreactivity among study population.
P53
nuclear positivity, as observed in Figure 8.1 (IHC), signifies the presence of
the p53 protein within the cell nuclei. In this context, p53 nuclear positivity
suggests that the p53 protein is actively present and localized within the
nuclei of the cells in the examined tissue sample. This finding can be
significant in cancer research and diagnosis, as alterations or overexpression
of the p53 protein are associated with various cancer types and can provide
insights into the molecular characteristics of the tumor, its prognosis, and
potential therapeutic implications. Therefore, identifying p53 nuclear
positivity through IHC analysis is vital in comprehending the biology and
behaviour of cancer cells in the context of the studied tissue or tumor
specimen.
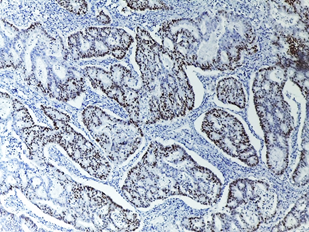
Figure 8.1. p53 nuclear
positivity corresponding to Image 1 (IHC).
In
table 1, the study revealed a noteworthy association between p53 expression and
various clinical-pathological characteristics. Notably, p53 positivity was more
frequent in moderately differentiated tumor grades compared to well and poorly
differentiated tumors. There was also a significant link between p53 expression
and tumor extension, with T3 and T4 tumors showing higher p53 positivity
compared to T1 and T2. Similarly, lymph node status and tumor stage exhibited
significant associations with p53 expression, indicating that N1 and N2 lymph
node statuses and stages S2 and S3 were more likely to be p53-positive.
However, no noteworthy links were observed between p53 expression and other
clinicopathological factors like age, sex, site of lesion, or tumor type.
Table 1. Correlation of
clinicopathologic parameters with the expression of p53.
|
Clinical pathological Characteristic |
Fisher’s Exact Value |
P-Value |
Association with p53 Expression |
|
Grade of the
Tumor |
7.255 |
0.024 |
Significant |
|
Moderately > Well & Poorly |
|||
|
Tumor
Extension |
5.355 |
0.031 |
Significant |
|
T3 & T4 > T1 & T2 |
|||
|
Lymph Node
Status |
7.177 |
0.012 |
Significant |
|
N1 & N2 > N0 |
|||
|
Stage of the
Tumor |
14.053 |
0.000 |
Significant |
|
S2 & S3 > S1 |
Discussion
The findings of our study provide valuable insights
into the clinicopathological characteristics and p53 expression in colorectal
adenocarcinoma cases within our patient population. The study discusses age distribution
in Figure 1 depicts a diverse age distribution, with a significant
representation in the 61-70 years age category. The male-to-female ratio of
0.8:1, as illustrated in Figure 2, aligns with existing literature. These
demographic observations are consistent with previous studies, mean age
distribution in previous studies ranged from 55.23 to 59 years, with varying
gender ratios, while our study showed a predominance of females, consistent
with study by (Mardi et al., 2017) (4). In this study Figure 3 highlights a
predilection for tumor growth on the left side of the colon and rectum,
consistent with known distribution. Clinical presentations varied, encompassing
symptoms such as abdominal pain, rectal bleeding, altered bowel habits, signs
of intestinal obstruction, weight loss, and anemia.
Histological grading, showcased in Figure 4, reveals a
predominance of adenocarcinoma NOS, with moderately differentiated tumors being
the most prevalent. Figure 5 illustrates diverse tumor extension patterns, with
a notable frequency of infiltration beyond the muscularis propria (T3). Figure
6 indicates diverse lymph node status, with notable associations in half of the
cases, and Figure 7 portrays a varied distribution of tumor staging, with Stage
II being the most frequently observed. In
our investigation, colorectal carcinomas were primarily classified as
adenocarcinoma NOS, with a predominance of moderately differentiated tumors,
followed by well-differentiated and poorly differentiated subtypes. The T
staging system revealed diverse tumor extension patterns, ranging from
infiltration beyond the muscularis propria (pT3) to confined muscularis propria
involvement (pT2), as well as infiltration into the visceral peritoneum or
adjacent organs (pT4) and rare early-stage T1 tumors, while lymph node status
and tumor stage indicated significant prognostic variability, with Stage II
being the most common, followed by Stage I and Stage III.
Moderately differentiated
adenocarcinoma displayed a higher frequency of p53 positivity (95.8%) compared
to well-differentiated tumors, with a statistically noteworthy link between p53
expression and tumor grade, consistent with findings (Harris & Hollstein, 2013) (5) reported an increased frequency of p53 expression in 95% of moderately
differentiated adenocarcinomas, further supporting this correlation.
Our study revealed a predilection for tumor growth on
the left side of the colon and rectum, a finding consistent with the known
distribution of colorectal cancers. (Fearon & Vogelstan, 2010) (6).
reported a comparable histological type distribution to our study, where
conventional adenocarcinomas were predominantly located in the left colon,
consistent with existing literature, and most cases in our study were
moderately differentiated (57.1%), in line with the findings by (Dignam et al.,
2016) (7).
The evaluation of lymph nodes continues to be the
primary method for determining prognosis and determining the need for adjuvant
treatment. We noted LNM in 21 cases (50%) which was comparable to the
investigation by (Chithra et al., 2018)
(8).
Similarly, Kim et al.,(2022) (9) summarize the role of
p53 signaling in colorectal cancer, including the molecular mechanisms, the
clinical implications, and the therapeutic strategies results have reported a high frequency of p53 expression
in colorectal carcinomas and its association with tumor grade, extension, lymph
node status, and stage. Another study
by (Cotran et al., 2014) (10) compares the clinical effect of p53 expression
and TP53 variation status in colorectal cancer patients, using
immunohistochemistry and next-generation sequencing hence finding suggest that p53 expression rather than TP53 variation
status has more significant impact on the overall survival of colorectal cancer
patients and also suggest However, some studies have also found significant
correlations between p53 expression and age, sex, lesion site, or tumor type , which were not observed in our study.
Another relevant stud done by Tomicic et al., (2021)
(11) which investigates the role of mutant p53 in colon cancer, using human and
mouse genetic studies and explain the possible mechanisms and functions of
mutant p53 in colorectal carcinogenesis and progression. Additionally, a study
done by Scott et al., (2011) (12) explores the epigenetic alterations upstream
and downstream of p53 signaling in colorectal cancer, including DNA
methylation, histone modifications, and micro-RNAs, insights into the complex regulation
of p53 signaling by epigenetic factors and its implications for colorectal
cancer diagnosis and therapy.Finally, study by Mizuho et al.,(2019) (13) which
examines the correlation between p53 expression and clinicopathological
parameters in colorectal cancer, using immunohistochemistry and corroborate
with current finding that p53 expression is associated with tumor grade,
extension, lymph node status, and stage in colorectal cancer patients.
Similarly, overexpression was observed in cases with
LNM (100%), indicating a poor prognosis associated with p53 detection in CRC. A
statistically noteworthy link was
found between p53 expression, tumor extension, and LNM. In Figure 8, p53
immunoreactivity is detected in 83.3% of cases, with a notable nuclear
positivity (Figure 8.1). Table 1 underscores significant associations between
p53 expression and clinicopathological characteristics, emphasizing its
prevalence in moderately differentiated tumors, advanced tumor stages, and
lymph node involvement. Our findings offer a comprehensive understanding of the
clinicopathological landscape of colorectal adenocarcinoma, highlighting the significance
of p53 expression as a potential prognostic indicator. These insights
contribute to the ongoing efforts to unravel the complexities of this
malignancy and pave the way for targeted therapeutic interventions. According
to study by (Dabiri et al., 2019) (14)
contributes to a comprehensive understanding of the clinicopathological
landscape of colorectal adenocarcinoma. The prevalence of p53 expression in
specific tumor grades and stages emphasizes its potential as a prognostic
marker. These insights not only validate prior research but also add nuanced
details to the intricate interplay between p53 and the progression of
colorectal carcinoma.Similarly (Russo et al., 2012)(15) observed associations
underscore the significance of p53 expression as a potential prognostic
indicator in colorectal adenocarcinoma. Identification of p53 as a molecular
marker holds promise for predicting the behavior of tumors and guiding
therapeutic interventions. Given its prevalence in advanced stages and lymph
node involvement, p53 expression could aid in risk stratification and
decision-making regarding the intensity of therapeutic strategies.
In summary of the discussion, the findings highlight
the diversity within CRC cases and underscore the significance of p53 as a
molecular marker associated with various clinicopathological parameters. The
clinical significance of p53 expression in colorectal carcinomas remains
debated, with our study suggesting its potential as a useful biomarker for
identifying advanced disease. Recent studies also support the role of p53
signaling in colorectal cancer and its impact on overall survival.
In study provides valuable data on clinicopathological
characteristics and p53 expression in colorectal adenocarcinoma, shedding light
on potential prognostic markers and guiding further research for a
comprehensive understanding of this complex disease
Conclusions
In
conclusion, study includes 42 colorectal adenocarcinoma cases providing key
insights. Notably, the age span (45-82 years) centers around 61-70 years, with
a male-to-female ratio of 0.8:1. Carcinoma growth predominantly occurs on the
left side (57%), and most cases are adenocarcinoma NOS (95.2%), with 57.1%
being moderately differentiated. Tumor extension, lymph node involvement, and
staging patterns exhibit diversity. P53 expression is detected in 83.3% of
cases, emphasizing its significant nuclear presence. Clinical-pathological
associations highlight links with tumor characteristics but not with age, sex,
site, or tumor type. Hence understanding of colorectal adenocarcinoma, with a
particular focus on the prevalent expression of p53 and its clinicopathological
implications. This underscores the importance of incorporating p53 status into
the comprehensive management strategy for this intricate malignancy.
Future
perspectives
Undoubtedly,
the reactivation and restoration of p53 function hold significant promise as a
novel therapeutic approach for CRC. However, it's worth noting that while
several molecules have demonstrated the ability to induce cell cycle arrest and
apoptosis in CRC cells, most of these findings originate from cell line and
animal model studies and have not yet progressed to clinical trials.
Additionally, the diverse oncogenic effects of mutant p53 remain incompletely
understood, and the impact of different mutations on p53 function complicates
the assessment of small molecule inhibitors targeting mutant p53 in clinical
trials. This area of research warrants further exploration. Notably, addressing
resistance to treatments and improving the prognosis of CRC patients with new
p53 mutations will necessitate the ongoing development of agents specifically
targeting these novel mutations.
Author
contribution
All
authors have contributed equally and read and approved the final draft of the
manuscript.
Conflict
of interest
The
authors report no conflict of interest.
References
1. Bernard W, Stewart PK, editors. World
Cancer burden. Lyon: IARC Press; 2013. pp. 16–17.
2. Parkin DM, Ferlay J, Hamdi-Cherif H, Sitas
F, Thomas JO, Wabinga H, Whelan SL. Cancer in Africa. IARC Press Lyon; 2010.
pp. 277–280.
3. Gondos A, Brenner H, Wabinga H, Parkin DM.
Cancer survival in Kampala, Uganda. Br J Cancer. 2015;92:1808–1812.
4. Mardi K, Sharma M, Bhardwaj M, Rao M. P53
Expression in Colorectal Carcinomas and Its Correlation With
Clinicopathological Parameters. Clin Cancer Investig J. 2017;6(1):26.
5. Harris Curtis C., Hollstein M. Clinical
implications of the p53 tumor suppressor gene. New Eng J of Med.
2013;329:1318–1327.
6. Fearon ER, Vogelstan B. Genetic model for
colorectal Tumorigenesis. Cell. 2010;61:759–767.
7. Dignam JJ, Ye Y, Colangelo L, Smith R,
Mamouncs EP, Wie HS, Wolmark N. Prognosis after rectal cancer in blacks and
whites participating in adjuvant therapy. Clin Oncol. 2016;21:413–420.
8. Chithrra V, John JJ, Ganapathy S, Raja V.
Immunohistochemical Study of p53 Expression in Colorectal Adenocarcinomas and
its Clinicopathological Correlation. Ann Pathol Lab Med. 2018;5(6):A521-526.
9. Kim, K.M., Ahn, AR., Park, H.S. et al.
Clinical significance of p53 protein expression and TP53 variation status in
colorectal cancer. BMC Cancer 22, 940 (2022).
https://doi.org/10.1186/s12885-022-10039-y
10. Cotran R, Kumar V, Collins T. Pathological
basis of disease. 7 ed. Philadelphia: W.B and Saunders; 2014. p. 864.
11. Tomicic, Maja T., Mona Dawood, and Thomas
Efferth. 2021. "Epigenetic Alterations Upstream and Downstream of p53
Signaling in Colorectal Carcinoma" Cancers 13, no. 16: 4072.
https://doi.org/10.3390/cancers13164072
12. Scott, N., Sagar, P., Stewart, J. et al. p53
in colorectal cancer: clinicopathological correlation and prognostic
significance. Br J Cancer 63, 317–319 (2011).
https://doi.org/10.1038/bjc.2016.74
13. Mizuho Nakayama, Masanobu Oshima, Mutant p53
in colon cancer, Journal of Molecular Cell Biology, Volume 11, Issue 4, April
2019, Pages 267–276, https://doi.org/10.1093/jmcb/mjy075
14. Dabiri Y, El Maaty MAA, Chan HY, Wölker J,
Ott I, Wölfl S, et al. P53-dependent anti-proliferative and pro-apoptotic
effects of a gold(I) N-heterocyclic carbene (NHC) complex in colorectal cancer
cells. Front Oncol. 2019;9(MAY):1–16.
15. Russo A, Bazan V, Iacopetta B, Kerr D, Soussi
T, Gebbia N. The TP53 Colorectal Cancer International Collaborative Study on
the Prognostic and Predictive Significance of p53 Mutation : Influence of Tumor
Site , Type of Mutation , and Adjuvant Treatment. 2021;23(30).