Psychometric
properties of the Persian version of the pain beliefs and perceptions inventory
(PBPI) in individuals with chronic low back pain
Sarvenaz Karimi-GhasemAbad 1,2,
Behnam Akhbari 3, Saeed Talebian Moghaddam 4, Ahmad
Saeedi 5
1 Razi Hospital, School of Medicine, Guilan University Medical
Sciences, Rasht, Iran
2 Physiotherapy Department of
University of Social Welfare and Rehabilitation Sciences, Tehran, Iran
3 Physiotherapy Department of University of Social Welfare and
Rehabilitation Sciences, Tehran, Iran
4 Physiotherapy Department of Tehran
University of Medical Sciences, Tehran, Iran
5 Department of Statistical Research
and Information Technology, Institute for Research and Planning in Higher
Education, Tehran, Iran
Corresponding Authors: Sarvenaz
Karimi-GhasemAbad
* Email:
s_karimi@gums.ac.ir
Abstract
Introduction: This study constitutes a methodological investigation
aimed at scrutinizing the validity and reliability of the Persian version of
the Pain Beliefs and Perceptions Inventory (PBPI) in individuals afflicted with
chronic low back pain.
Methods: To gauge reliability, both the test-retest and internal consistency
methods were deployed. Furthermore, the correlation coefficient was utilized to
assess discriminant validity among 118 individuals suffering from chronic low
back pain. The questionnaire's construct validity was ascertained by probing
the correlation between the subscales of pain persistence in the future, pain
stability in the present, self-blame, and the mysteriousness of pain, with the
constructs of pain catastrophizing, disability, pain-related anxiety, coping
strategies, quality of life, and pain intensity.
Results: Statistical analysis using the Shapiro-Wilk test revealed a non-normal
data distribution. Consequently, the non-parametric Spearman's correlation
coefficient was used to scrutinize construct and discriminant validity. The
intraclass correlation coefficient (ICC) ranged from 0.58 to 0.78 for the
subscales of pain persistence in the future, pain stability in the present,
self-blame, and the mysteriousness of pain. Additionally, Cronbach's alpha
coefficient ranged from 0.74 to 0.88. With the exception of the self-blame
subscale, the other subscales exhibited significant positive correlations with
constructs of pain catastrophizing, disability, anxiety, coping strategies, and
pain intensity, as well as significant negative correlations with quality of
life (correlation coefficient ranging between 0.19 and 0.49).
Conclusion: The outcomes about test-retest reliability, construct validity, and
discriminant validity collectively suggest that the Persian version of the PBPI
possesses robust psychometric properties.
Keywords: Pain Beliefs and Perceptions Inventory, Chronic Low Back Pain,
Validity, Reliability
Introduction
Chronic back pain is one of the most common
musculoskeletal disorders with a prevalence of 10-20%. Evidence reveals the
influential role of socio-demographic, psychological, and clinical
characteristics in the chronicity of back pain (1). Examining psychological
risk factors, in addition to the biomechanical approach, aids us in our
understanding of the persistence and spread of back pain (2).
Back pain is not always associated with movement
disorders and abnormalities. Sometimes, there is an association with negative
effects on social relationships, life satisfaction, and psychological disorders
such as depression and anxiety. The profile of psychosocial performance in
people suffering from back pain is related to their type of pain perception,
coping strategy and level of social support (3).
The biopsychosocial model of pain considers the type of
pain perception and coping strategies as two factors that can explain the
difference between individuals with chronic pain. A person’s belief toward pain
and the way they perceive it, along with their coping strategies can differ,
depending on the situation and culture (4, 5). Research suggests that
unfavorable attitudes about pain have an impact on how well chronic pain is
treated. Unfavorable attitudes can also turn acute pain into chronic pain and have
a detrimental effect on a patient's overall health, self-efficacy, and
performance (5, 6). It is recommended that individuals with chronic pain use a
variety of cognitive-behavioral techniques to address maladaptive beliefs (6).
Different tools were designed to evaluate and determine the beliefs related to
pain. The Pain Beliefs and Perceptions Inventory (PBPI) is one of them. Quick
and easy identification of cognitive factors is one of the reasons for choosing
this scale. This 16-item instrument was designed by Williams and Thorn in 1989.
Each of its statements is rated, using a 4-point Likert scale including options
of strongly agree, agree, disagree, strongly disagree (7). The PBPI evaluates
emotions, behavior, and pain-related perceptions. Strong relationships have
been found between this tool and personality traits, physiological processes,
coping mechanisms, and feelings of anxiety, depression, and pain (8).
The original version of the questionnaire is
composed of three factors namely, time (belief in the stability and continuity
of pain), mysteriousness (belief in the mysteriousness and unknowingness of
pain) and self-blame (self-guilt and blaming oneself for the pain). The study
found that the internal consistency coefficients for the time and
mysteriousness of pain subscales as well as self-blame were 0.65 and 0.80,
respectively (7). According to a study by Turner et al. (2000) on patients with
chronic pain, those who believe in persistence of their pain in the present and
continuation of it in the future are more likely to experience physical
disability and depression with more severity. The lack of repetition of the
time factor, and the emergence of two factors of belief in pain permanence and
pain constancy led to the design of a four-factor model (9). Asghari et al.
(2005) investigated the psychometric properties of this questionnaire among 232
patients with cancer pain. In this study, the construct validity of the
questionnaire was tested using the factor analysis method, and the fourth
statement (pain confuses me) was removed from the factor analysis due to a very
strong positive bias (10).
The first factor is belief in Pain Permanence with a
score between 8 and -8. A positive score indicates a deeper belief in the
continuation of pain in the future. The second factor is self-blame. Its score
is between 6 and -6, with a positive score suggesting a deeper belief in
self-blame. Pain Constancy is stated as the third factor. Its score ranges from
8 to -8. A positive score in this situation expresses a deeper belief in the
stability of pain. The fourth and final factor is Mysteriousness, scoring between
8 and -8. A higher score shows a deeper belief in the unknowability of pain and
a person's attitude towards pain as an ambiguous phenomenon. The internal
consistency coefficients of these four factors varied between 0.70 and 0.77.
Persian version of PBPI questionnaire has a significant correlation with
disability, psychological structures and coping strategies (10).
The PBPI questionnaire has been translated into several
languages with different target populations (6, 11-15). Although the Persian
version of this questionnaire is available, due to the different nature of
chronic cancer pain and chronic musculoskeletal pain, the psychometric
characteristics of the Persian version have not been investigated among people
with chronic low back pain. Therefore, the aim of the present study is to
investigate the validity and reliability of the Persian version of PBPI among
this group of patients. Based on the COSMIN checklist, the following hypotheses
were considered to express the correlation between the PBPI questionnaire and
other scales (16).
1. There is a positive and significant correlation
between the subscales of the PBPI questionnaire and the constructs of pain
catastrophizing, Roland Morris disability questionnaire, coping mechanisms,
pain-related anxiety symptoms and pain intensity of people dealing with chronic
back pain.
2. There is a negative and significant correlation
between the subscales of the PBPI questionnaire and the quality of life of
people with chronic back pain.
Methods
This study of localization, validity and reliability of
PBPI scales is a methodological one. 118 people suffering from chronic back
pain who visited the physical therapy centers of Tehran in the summer and fall
of 2017 and 2018 participated in this study (15). The criteria for entering the
study include: suffering from back pain for more than three months, the ability
to speak Farsi (Persian language), and being in the age range of 18 to 55 (17).
People with cognitive disorders, known pathologies (such as discopathy, spinal
canal stenosis, fractures in the spine and osteoporosis), and spondylolisthesis
as well as those who were pregnant were excluded from the study (17).
Eventually, 118 people were eligible to participate in the study and all of
them signed the participation consent form. This study was approved by the
Ethics Committee of The University of Social Welfare and Rehabilitation
Sciences (No:IR.USWR.REC.1396.205).
Pain Beliefs
Perception Inventory (PBPI)
The questionnaire was designed by Williams and colleagues
in 1989 to assess people with chronic non-cancer pain. The original version of
this questionnaire has 16 items and three subscales including mystery, time,
and self-blame. Patients rate their pain beliefs on a four-point Likert scale
from -2 (completely disagree) to +2 (completely agree). The scoring of 3, 9, 12
and 15th items are calculated in reverse (7). After the factorial structure of
the PBPI was examined, four factors (mystery, permanence, constancy, and
self-blame) were ultimately identified (9).
Asghari et al. localized this questionnaire in Persian language in 2005,
which resulted in 15 items with four similar subscales (10). The factor of
belief in pain permanence in the future is obtained through summation of the
scores achieved from statements Nos. 4, 8, 11 and 14. Summing up the scores of
statements Nos. 6, 10 and 12 presents us with the factor of belief in
self-blame. Moreover, the score from statements Nos. 5, 3, 9 and 15, states the
factor of belief in the constancy of pain in the present time. The factor of
belief in the mystery of pain is obtained from the sum of the scores related to
statements Nos. 2, 1, 7 and 13.
Coping
Strategies Questionnaire (CSQ-8)
The CSQ questionnaire was designed by Rosenstiel and
Keefe (1983) in people with chronic back pain. This tool had 50 items, 7
diverse cognitive and behavioral strategies. The six mentioned cognitive
strategies include diverting attention, catastrophizing, ignoring pain
sensations, reinterpretation, coping self-statements, and praying. It is
considered a behavioral coping strategy to increase the level of activity.
Behavioral and cognitive coping strategy scales of each item have seven options
(0 = never use, 3 = sometimes use, 6 = always use) (18). Each scale is scored
between 0 and 36. The Persian version of this scale is available, which,
similar to the original version, has Cronbach's alpha coefficient of above 0.70
for subscales (19).
Roland Morris
Disability Questionnaire (RMDQ)
This questionnaire is used to measure the disability
caused by chronic back pain. It contains 24 questions with yes and no answers.
Its score is from 0 to 24, where 0 indicates no disability and 24 indicates
severe disability. This scale is widely used in various researches and has
favorable internal consistency and construct validity (20).
Visual Analog
Scale (VAS)
Visual analog scale is used to measure pain intensity.
This scale includes a straight horizontal line of 100 mm, with one end being
"no pain" and the other being "the most severe pain
possible". The patient marks the pain intensity on the 100 mm continuum of
this straight line (21).
Pain
Catastrophizing Scale (PCS)
The scale of pain catastrophizing was designed by
Sullivan (1995) with the aim of evaluating the level of catastrophic thoughts
and behaviors of a person (22). In this questionnaire, subjects are asked to
reflect on past painful experiences. Then, rate the degree they experience the
thirteen mentioned thoughts and feelings during these events on a 6-point
scale. The scale ranges from 0, "not at all or at all" to 4,
"always or always" (23).
Beck Depression
Inventory-II (BDI-II)
This questionnaire was first designed by Beck. Today, its
21-item version is used which includes specific symptoms of depression. The
samples are selected with one of these items that indicates the severity of
depression symptoms (24). Each item has a score between 0 and 3. The total
score is between 0 and 63. This questionnaire can be used in people over 13
years old and it was localized by Ghasemzadeh in 2005. Its Cronbach's alpha was
reported as 0.87 (25).
Pain Anxiety
Symptom Scale (PASS-20)
Pain Anxiety Symptom Scale is a self-report tool designed
by McCracken in 1992. It is deployed to assess anxiety and fear reactions
caused by pain in people who suffer from chronic pain. The total score is
between 0 and 100. A higher score indicates pain-related anxiety (26).
Shanbezadeh et al (2017) scrutinized the validity and reliability of this tool
among the chronic back pain group. Intraclass correlation coefficients for all
subscales were higher than 0.70%. Also, Cronbach's alpha was more than 0.70% for
all the subscales (27).
Short Form-36
(SF-36)
The quality-of-life scale, a shortened 36-itemed form,
was designed by Ware (1992) to evaluate the quality of life and general health
(28). This questionnaire was translated into Farsi in 2005 and its psychometric
properties were examined (29).
Statistical
Analysis
Ceiling and floor effects determine the number and
percentage of people who got the lowest and highest score in each of the
subscales. If more than 15% of patients have a minimum or maximum score, the
questionnaire cannot differentiate between patients at the extremes of the
scale (30) .
To evaluate the reliability, this scale was given to 54
patients with chronic back pain in two stages, with a time interval of one
week. The purpose of retest assessments was to differentiate between actual
score variance and temporary error, which arises from time-related variations
in individuals' emotional states, physiological conditions, or cognitive
processes (31). In order to measure relative and absolute reliability,
Intraclass correlation coefficient (ICC), Standard error of measurement (SEM) and
Minimal detectable change (MDC) were calculated between the two stages of
measurement (32). By using absolute reliability indices, it is possible to
distinguish clinical changes in the sample's condition from changes that may be
due to measurement error. To calculate ICC in SPSS version 17, Two-Way
Random-Effects Model or (1 and 2) was used.
ICC equal to or higher than 0.7 was considered as the
acceptable limit of the reliability level. SEM was obtained using ICC and
standard deviation, and MDC was obtained using SEM, with its calculation
formula stated as below (33):
![]()
![]()
Internal consistency reliability was assessed with
Cronbach’s Alpha on the 4 subscales of the PBPI, which is used to evaluate the
strength of the relationship between individual's questions within the scale.
Mean scores, an alpha coefficient of more than 0.80 was considered as sufficient
and acceptable (32).
The Bland-Altman analysis was used to assess how well
subscales agree between tests and retests. The mean difference and limits of
agreement with a 95% confidence interval served as the method's outcome
measures (17).
To evaluate the construct validity of the Persian version
of the PBPI scale, the correlation between the score of their subscales and the
scores of the Persian version of RDMQ, PCS, CSQ, CSQ, PASS-20, SF-36 and pain
intensity was calculated in people with non-specific chronic back pain.
In order to calculate the Item-Total correlation,
Dimensionality on an item level, after individually removing the score of each
item from the subscale score related to it, Spearman's correlation coefficient
was measured for each item with its corresponding subscale score. Acceptable
correlation coefficients are 0.4 or lower, and each item's correlation with
each of the other subscales should be less than that of the relevant subscale
(34).
Results
The background information of people was collected
through a self-report questionnaire designed by the researcher. The average age
of the subjects was 36.36 with a standard deviation of 10.51 years. The average
pain intensity during the test was 30.9 mm based on the linear scale. 29.2% of
the subjects in this research were men and 70.8% were women. 19.1% of subjects
had education up to diploma, 48.4% had bachelor's degree and 32.5% had master's
and doctorate education. The results of the Shapiro-Wilk statistical test
showed that the distribution of data in all subscales of the PBPI questionnaire
was not normal. Therefore, in the present study, non-parametric statistical
methods were used to check the correlation of data.
Table 1 shows the floor and ceiling effect for the
subscales’ scores of the Persian version of PBPI. As can be seen in the table,
less than 15% of people had the minimum or maximum scores of the subscales,
except the self-blame subscale.
The obtained results from ICC, SEM, MDC and Bland-Altman
agreement along with the mean and standard deviation of each subscale are also
mentioned in Table 1. Munro's classification was used to describe the degree of
relative reliability (17).
Reliability between zero and 0.25 was considered very
low, 0.26 and 0.49 low, 0.50 and 0.69 medium, 0.7 and 0.89 high, and finally,
0.9 and 1 very high. For the majority of the subscales, ICC values between 0.70
and 0.78 were found, which is above the acceptable limit. However, for the
subscale of belief in the mystery of pain, an average score of 0.58 was
reported. According to Table 1, Cronbach's alpha values in this study for the
subscales’ scores ranged from 0.74 to 0.88.
Table
1. Flooring
and ceil effects, Test-retest reliability, limitation of agreement of Persian
version of PBPI (n=118).
|
SUBSCALE |
Permanence |
Self-blame Pain |
Constancy |
Mysteriousness |
|
mean |
-6.23 |
0.26 |
-2.85 |
-1.25 |
|
SD |
5.58 |
3.13 |
3.2 |
3.02 |
|
Cronbach’s
alpha |
0.82 |
0.83 |
0.88 |
0.74 |
|
ICC |
0.70(0.53-0.81) |
0.72(0.56-0.83) |
0.78(0.65-0.9087) |
0.58(0.38-0.73) |
|
SEM |
3.05 |
1.65 |
1.5 |
1.95 |
|
MMDC |
8.47 |
4.59 |
4.16 |
5.42 |
|
flooring
effect % |
0.80% |
3.40% |
1.70% |
3.40% |
|
ceiling
effect% |
2.50% |
28% |
4.20% |
1.70% |
|
mean
difference (95% CI) |
-0.301 (-1.47-0.87) |
0.37 (-0.635-0.71) |
-0.339 (-0.93-0.25) |
0.43 (-0.34-1.21) |
|
LOA |
-8.67-8.07 |
-4.74-4.82 |
-4.58-3.9 |
-5.08-5.95 |
SD: standard deviation, ICC: intraclass correlation
coefficient, SEM: Standard Error of Measurement, MDC: minimal detectable
change, LOA: limitation of agreement.
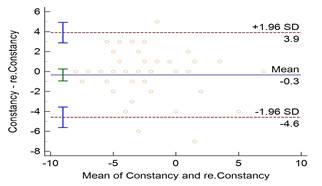
Figure
1.
Bland-Altman Plot of constancy subscale of Persian version of PBPI in
individual with non-specific Chronic Low Back pain.
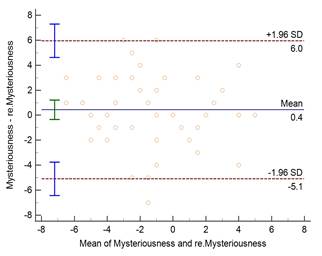
Figure
2. Bland-Altman
Plot of Mysteriousness subscale of Persian version of PBPI in individual with
non-specific Chronic Low Back pain.
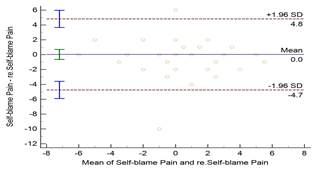
Figure
3. Bland-Altman
Plot of self-blame subscale of Persian version of PBPI in individual with
non-specific Chronic Low Back pain.
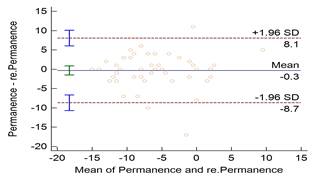
Figure
4. Bland-Altman
Plot of Permanence subscale of Persian version of PBPI in individual with non-specific
Chronic Low Back pain.
The correlation coefficients between the subscales’
scores of the PBPI questionnaire with the scores of the RMDQ, CSQ, PCS,
PASS-20, SF-36 and pain intensity are summarized in table 2.
Table
2. Correlation
coefficients between PBPI questionnaire scores with RMDQ, CSQ, BDI-II, PCS,
PASS-20, SF-36 questionnaire scores and pain intensity (n=118).
|
Scales/ subscales |
Permanence |
Self-blame Pain |
Constancy |
Mysteriousness |
|
PCS |
0.424** |
0.139 |
0 .361** |
0.332** |
|
PASS.20 |
0.353** |
0.110 |
00.266** |
0.230* |
|
BDI-II |
0.416** |
0.073 |
0 .367** |
0.266** |
|
SF36.PH.T |
-0.511** |
-0.021 |
-0.500** |
-0.306** |
|
SF36.MH.T |
-0.323** |
-0.069 |
-0.237* |
-0.269** |
|
SF36.T |
-0.455** |
-0.050 |
-0.401** |
-0.315** |
|
Diverting
attention |
-0.027 |
0.076 |
0.031 |
-0.102 |
|
Reinterpretation |
0.025 |
.192* |
0.054 |
-0.006 |
|
Catastrophizing |
.500** |
0.150 |
0.398** |
0.300** |
|
Ignoring
pain |
-0.198* |
0.137 |
-0.118 |
-0.061 |
|
Praying-hope |
0.110 |
0.075 |
0.154 |
-0.007 |
|
self-statement |
-0.074 |
0.141 |
0.050 |
-0.167 |
|
Increasing
activity levels |
0.023 |
0.182 |
0.093 |
0.088 |
|
VAS. |
0.212* |
0.147 |
0.194 |
0.062 |
|
RMDQ |
0.462** |
0.172 |
0.482** |
0.190* |
**
Correlation coefficients significant at P<0.000, *Correlation coefficients
significant at P<0.05. PCS; Pain Catastrophizing Scale, VAS; Visual Analogue
Scale, RMDQ; Roland Morris Disability Questionnaire; BDI-II; Back Inventory
Index, SF-36; Short Form, MH; Mental Health, PH; Physical Health, PASS; Pain
Anxiety Symptom Scale, Pain Intensity.
The results of Table 3 shows that the Spearman
correlation between each item and its corresponding subscale was between 0.360
and 0.689, whereas the correlation with other subscales was between 0.089 and
0.589. This means that the correlation of each item with its own subscale was
more than the correlation between the score of that item with other subscales.
A significant value for the correlation between all items and subscales was
reported to be less than 0.001.
Table
3. Item-total
correlation of Persian version of PBPI (n=118).
|
Item |
Permanence |
Self-blame Pain |
Constancy |
Mysteriousness |
|
I4 |
0.689** |
0.259** |
0.616** |
0.399** |
|
I8 |
0.399** |
0.019 |
0.311** |
0.143** |
|
I11 |
0.454** |
0.002 |
0.326** |
0.377** |
|
I14 |
0.461** |
0.072 |
0.333* |
0.243* |
|
I6 |
0.12 |
0.684** |
0.123 |
0.038 |
|
I10 |
0.057 |
0.658** |
0.027 |
-0.009 |
|
I12 |
0.213* |
0.36** |
0.123 |
0.116 |
|
I3 |
0.608** |
0.037 |
0.578** |
0.207* |
|
I5 |
0.654** |
0.035 |
0.584** |
0.256** |
|
I9 |
0.701** |
0.015 |
0.602** |
0.248** |
|
I15 |
0.667** |
0.059 |
0.478** |
0.357** |
|
I1 |
0.037 |
0.197* |
0.801** |
0.551** |
|
I2 |
0.061 |
0.333** |
0.654** |
0.636** |
|
I7 |
0.081 |
0.289** |
0.744** |
0.512** |
|
I13 |
-0.131 |
0.186 |
0.677** |
0.486** |
Discussion
In the current study, less than 15% of the participants
met the minimum and maximum scores in the subscales, with the exception of
self-blame, which had a floor impact of 0.28%. This can show the power of the
Persian version of the PBPI scale in differentiating the various beliefs and
pain perception in patients with back pain. Findings from the current study
corroborated results from a research by Monticone et al. (2014) and Azevedo et
al. (2017), where more than 15% of individuals had at least a minimal score on
the self-blame subscale. (6, 15).
All subscales' ICC values fell between 0.7 and 0.78, with
the exception of the mystery of pain subscale, which had a score of 0.58. This
result validates the average of the mystery of pain subscale and the other
three subscales' strong reliability. It also shows that in both tests, the
order of people with respect to the entire test group has stayed appropriate.
The results of another study including individuals with chronic pain fell
within a same range (0.88-0.79) (15). The results of the other research, which
included participants with chronic back pain, were similar (6). Cronbach's
alpha coefficient of the subscales of mystery of pain was reported to be in the
range of 0.74 to 0.88, which is in line with the results of other studies that
had been done previously (6, 10, 15).
The minimum MDC for the subscales of belief in pain
permanence, self-blame, pain constancy, and mysteriousness were 89.47,4.59,
4.16, and 5.42, respectively. With the aid of the MDC results, therapists and
researchers are able to ascertain the true changes and validity of the
subscales' scores (27). The agreement between the mean difference and the
results indicates that each subscale fell within the predetermined limitations.
Failure to calculate MDC and SEM and agreement in previous studies has limited
the possibility of comparing their results.
The PBPI subscales' construct validity results suggested
that, all subscales, except self-blame exhibited a positive and significant
association with disability, pain-related anxiety symptoms, depression, and
catastrophizing. Also, a significant negative relationship was observed between
the quality of life and the subscales of pain permanence, pain constancy, and
pain mystery. Among the coping strategies, only catastrophizing showed a
positive and significant relationship with three subscales of the PBPI questionnaire,
except self-blame. A positive and significant relationship was reported between
pain intensity and the subscales of pain
among 122 people with chronic pain. A negative
relationship was observed between the level of quality of life and the
subscales of pain mystery, pain constancy, and pain permanence. Similar to the
present study, they did not report a significant relationship between this
questionnaire and the subscale of self-blame (15).
A notable positive correlation was observed between the
permanence subscales and pain intensity, while no such association was
identified for the remaining subscales. The permanence subscales of the PBPI
concentrate on the daily life encounters of pain, suggesting a potentially more
robust connection with the factual experience of pain intensity as assessed
through the VAS. Contrary findings were reported by Blanch et al., who
evidenced a strong correlation between all PBPI subscales and pain intensity.
Discrepancies in results may be attributed to variations in sample sizes;
notably, the study by Blanch et al. predominantly involved participants
afflicted with fibromyalgia (8).
According to the Cognitive-Behavioral Theory and the
Biopsychosocial model, there is a significant correlation between disability,
pain catastrophizing, and predictable coping strategies (8). This statement
confirms the results of previous studies as well as the present one. The lack
of correlation between self-blame and other scales was also found in previous
studies. This could be due to the lack of a structure related to self-blame,
which calls for more attention in future studies (1, 13, 35, 36). The construct
validity results confirmed the hypotheses considered at the beginning of the
present research.
The strong correlation between the items of the Persian
version of PBPI with their corresponding subscale indicates the appropriate
structure of this version. In addition, it shows that each subscale consists of
appropriate items (6, 15).
Limitation
This
study's limited number of participants may compromise its external validity and
generalizability. Moreover, lack of implementation of content validity and
exploratory factor analysis is another limitation that can be addressed in
future studies.
Conclusion
The psychometric properties of the Persian version of the
Pain Beliefs and Perceptions Inventory (PBPI) were examined among individuals
suffering from chronic back pain, demonstrating commendable levels of validity
and reliability. This instrument can be effectively employed by physical
Therapists and researchers to assess patients' beliefs and perceptions
regarding pain, contributing to enhanced treatment outcomes.
Competing
interests
The authors declare that they have no competing interests.
Statement
of the Institutional Review Board Approval
Informed
consent form approved by the Ethics Committee at University of Social Welfare
& Rehabilitation Sciences (No: IR.USWR.REC.1396.205).
Authors
contributions
BA, STM and
AS contributed to the concept and design of the study and collected the
data. SKGA drafted the manuscript and prepared the final version, read
and revised the manuscript critically for important intellectual content.
Finally, all authors approved the final version of the manuscript for
publication.
References
1. Müller M,
Curatolo M, Limacher A, Neziri AY, Treichel F, Battaglia M, et al. Predicting
transition from acute to chronic low back pain with quantitative sensory
tests—A prospective cohort study in the primary care setting. European journal
of pain. 2019;23(5):894-907.
2. Gajsar H,
Titze C, Levenig C, Kellmann M, Heidari J, Kleinert J, et al. Psychological
pain responses in athletes and non‐athletes with low back pain: avoidance and
endurance matter. European Journal of Pain. 2019.
3. Misterska E,
Jankowski R, Glowacki M. Chronic pain coping styles in patients with herniated
lumbar discs and coexisting spondylotic changes treated surgically: Considering
clinical pain characteristics, degenerative changes, disability, mood
disturbances, and beliefs about pain control. Medical science monitor :
international medical journal of experimental and clinical research.
2013;19:1211-20.
4. Ferreira-Valente
MA, Pais-Ribeiro JL, Jensen MP. Psychometric properties of the portuguese
version of the Pain Self-Efficacy Questionnaire. Acta reumatologica portuguesa.
2011;36(3):260-7.
5. Tabriz ER,
Mohammadi R, Roshandel GR, Talebi R. Pain Beliefs and Perceptions and Their
Relationship with Coping Strategies, Stress, Anxiety, and Depression in
Patients with Cancer. Indian journal of palliative care. 2019;25(1):61-5.
6. Monticone M,
Ferrante S, Ferrari S, Foti C, Mugnai R, Pillastrini P, et al. The Italian
version of the Pain Beliefs and Perceptions Inventory: cross-cultural
adaptation, factor analysis, reliability and validity. Quality of life research
: an international journal of quality of life aspects of treatment, care and
rehabilitation. 2014;23(6):1789-95.
7. Williams DA,
Thorn BE. An empirical assessment of pain beliefs. Pain. 1989;36(3):351-8.
8. Blanch A,
Solé S. Classification of pain intensity with the pain beliefs and perceptions
inventory (PBPI) and the pain catastrophizing scales (PCS). Quality of life
research : an international journal of quality of life aspects of treatment,
care and rehabilitation. 2023;32(10):2853-9.
9. Turner JA,
Jensen MP, Romano JM. Do beliefs, coping, and catastrophizing independently
predict functioning in patients with chronic pain? Pain. 2000;85(1-2):115-25.
10. Asghari
Moghadam MA KN, Amarloo P. The role of beliefs about pain in adjustment to
cancer. Daneshvar Raftar. 2005(13):1-22.
11. Dysvik E,
Lindstrøm TC, Eikeland O-J, Natvig GK. Health-related quality of life and pain
beliefs among people suffering from chronic pain. Pain management nursing.
2004;5(2):66-74.
12. Williams DA,
Keefe FJ. Pain beliefs and the use of cognitive-behavioral coping strategies.
Pain. 1991;46(2):185-90.
13. Herda CA,
Siegeris K, Basler H-D. The Pain Beliefs and Perceptions Inventory: further
evidence for a 4-factor structure. Pain. 1994;57(1):85-90.
14. Wong WS,
Williams DA, Mak KH, Fielding R. Assessing attitudes toward and beliefs about
pain among Chinese patients with chronic pain: Validity and reliability of the
Chinese version of the Pain Beliefs and Perceptions Inventory (ChPBPI). Journal
of pain and symptom management. 2011;42(2):308-18.
15. Azevedo LF,
Sampaio R, Camila Dias C, Romão J, Lemos L, Agualusa L, et al. Portuguese
Version of the Pain Beliefs and Perceptions Inventory: A Multicenter Validation
Study. Pain practice : the official journal of World Institute of Pain.
2017;17(6):808-19.
16. Mokkink LB,
Terwee CB, Knol DL, Stratford PW, Alonso J, Patrick DL, et al. The COSMIN
checklist for evaluating the methodological quality of studies on measurement
properties: a clarification of its content. BMC medical research methodology.
2010;10(1):1-8.
17. Karimi-GhasemAbad
S, Akhbari B, Saeedi A, Moghaddam ST, Ansari NN. The Persian Brief Illness
Perception Questionnaire: validation in patients with chronic non-specific low
back pain. 2020.
18. Rosenstiel AK,
Keefe FJ. The use of coping strategies in chronic low back pain patients:
Relationship to patient characteristics and current adjustment. Pain.
1983;17(1):33-44.
19. Asghari A,
Golak N. The roles of pain coping strategies in adjustment to chronic pain.
Scientific Information Database (SID). 2005.
20. Mousavi SJ,
Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry disability index,
the Roland-Morris disability questionnaire, and the Quebec back pain disability
scale: translation and validation studies of the Iranian versions. Spine.
2006;31(14):E454-E9.
21. Price DD,
McGrath PA, Rafii A, Buckingham B. The validation of visual analogue scales as
ratio scale measures for chronic and experimental pain. Pain. 1983;17(1):45-56.
22. Sullivan MJ,
Bishop SR, Pivik J. The pain catastrophizing scale: development and validation.
Psychological assessment. 1995;7(4):524.
23. Raeissadat S,
Sadeghi S, Montazeri A. Validation of the pain catastrophizing scale (PCS) in
Iran. J Basic Appl Sci Res. 2013;3:376-80.
24. Beck AT, Steer
RA, Brown GK. Beck depression inventory-II. San Antonio. 1996;78(2):490-8.
25. Ghassemzadeh
H, Mojtabai R, Karamghadiri N, Ebrahimkhani N. Psychometric properties of a
Persian-language version of the Beck Depression Inventory--Second edition:
BDI-II-PERSIAN. Anxiety and Depression Association of America (ADAA).
2005;21(4):185-92.
26. McCracken LM,
Dhingra L. A short version of the Pain Anxiety Symptoms Scale (PASS-20):
preliminary development and validity. Pain Research and Management.
2002;7(1):45-50.
27. Shanbehzadeh
S, Salavati M, Tavahomi M, Khatibi A, Moghadam ST, Khademi-kalantari K.
Reliability and Validity of the Pain Anxiety Symptom Scale in Persian Speaking
Chronic Low Back Pain Patients. Spine. 2017.
28. Ware J, John
E, Gandek B. The SF-36 Health Survey: Development and use in mental health
research and the IQOLA Project. International Journal of Mental Health.
1994;23(2):49-73.
29. Montazeri A,
Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36):
translation and validation study of the Iranian version. Quality of life
research : an international journal of quality of life aspects of treatment,
care and rehabilitation. 2005;14(3):875-82.
30. Seydi M,
Akhbari B, Abad SKG, Jaberzadeh S, Saeedi A, Ashrafi A, Shakoorianfard MA.
Psychometric properties of the Persian version of the brief illness
questionnaire in Iranian with non-specific chronic neck pain. Journal of
Bodywork and Movement Therapies. 2021;28:323-31.
31. Polit DF, Yang
F. Measurement and the measurement of change: a primer for the health
professions: Wolters Kluwer Health; 2015.
32. Terwee CB, Bot
SD, de Boer MR, van der Windt DA, Knol DL, Dekker J, et al. Quality criteria
were proposed for measurement properties of health status questionnaires.
Journal of clinical epidemiology. 2007;60(1):34-42.
33. Seydi M,
Akhbari B, Abdollahi I, Abad SKG, Biglarian A. Confirmatory factor Analysis,
reliability, and validity of the Persian version of the coping strategies
questionnaire for Iranian people with nonspecific chronic neck pain. Journal of
Manipulative and Physiological Therapeutics. 2021;44(1):72-84.
34. Howard KI,
Forehand GA. A method for correcting item-total correlations for the effect of
relevant item inclusion. Educational and Psychological Measurement.
1962;22(4):731-5.
35. Morley S,
Wilkinson L. The Pain Beliefs and Perceptions Inventory: a British replication.
Pain. 1995;61(3):427-33.
36. Strong J,
Ashton R, Stewart A. Chronic low back pain: toward an integrated psychosocial
assessment model. Journal of consulting and clinical psychology.
1994;62(5):1058.