Glomangiopericytoma,
a rare sinonasal hemangiopericytoma with particular characteristics
Ehsan Arjmandzadeh 1, Abolfazl Taheri 2*
1 Shahid Sadoughi University of
Medical Sciences, Yazd, Iran
2 Baqiyatallah University of Medical
Sciences, Tehran, Iran
Corresponding Authors: Abolfazl Taheri
* Email: dr.abolfazl.taheri@gmail.com
Abstract
Introduction: Glomangiopericytoma (GPC) is an extremely rare
paranasal sinuses and nasal cavity vascular neoplasm introduced and
differentiated from the conventional hemangiopericytoma in 1998 by Granter et
al. Up to now, to the best of our knowledge less than 250 confirmed cases have
been reported in the literature. However, the exact etiology is unknown but
some risk factors including trauma, hypertension, long term steroid use and
pregnancy have been suggested as predisposing factors. Nasal obstruction is the
most common presentation followed by intermittent epistaxis, pain, proptosis
and epiphora.
Case presentation: Here we describe a case of right sided glomangiopericytoma that was
completely resected with safe margins by a Weber-Ferguson approach and
underwent adjuvant radiotherapy with no evidence of recurrence one year after
surgery.
Discussion: Although glomangiopericytoma is very rare but it should be considered
in case of confronting a unilateral vascular mass especially in pregnant
females with a history of hypertension, trauma or long-term steroid usage.
Definite diagnosis is based on immunohistochemistry and preoperative imaging is
mandatory as endoscopic approach should be kept for small sized tumors with
definitely identified origin.
Conclusion: Glomangiopericytoma is a rare tumor classified as a low-grade
borderline malignancy tumor. Complete excision and long term follow up due to
high rate of recurrence are required.
Keywords: Hemangiopericytoma, Paranasal sinuses and nasal cavity, Vascular
Neoplasm, Complete Excision
Introduction
Glomangiopericytoma
(GPC(,
is an extremely rare sinonasal vascular neoplasm which comprises less than 0.5
percent of all sinonasal neoplasia that introduced and differentiated from
hemangiopericytoma in 1998 by Granter et al and since then to the best of our
knowledge less than 250 confirmed cases have been reported in the literature
(1-3). This neoplasm differs from the conventional hemangiopericytoma in three
aspects, first the anatomical origin, GPC is usually seen in sinonasal tract,
second in biological behavior, GPC as in many reports is an indolent low
malignant potential neoplasm with excellent prognosis in case of complete
surgical resection but it’s potential for local invasion and metastatic spread
has been reported too, and finally the third difference is histopathological
features considering the fact that GPC originates from perivascular modified
smooth muscle cells with round, spindled and focally disposed whirling pattern
cells frequently expressing smooth muscle actin (SMA) and CD 34 in
immunohistochemistry assessments (4, 5). The tumor is very slightly female
dominant and although seen in all age groups, the peak incidence occurs during
the fifth and sixth decades of life and is usually presented with unilateral
nasal obstruction and/or epistaxis and facial pain or headache (3, 6, 7). In 2005 the WHO classification of head and
neck tumors proposed that sinonasal hemangiopericytoma should be named
glomangiopericytoma considering their similarity with glomus tumors (8).
Here
we describe a case of right-sided glomangiopericytoma, treated surgically with
open approach by a typical incision of Weber Ferguson.
Case
presentation
A
48-year-old man presented to our medical center with chief complaint of
complete right sided nasal obstruction. The obstruction process was progressive
with almost six weeks of partial obstruction that converted to complete
obstruction from two months ago. He felt a radicular sharp right hemifacial
pain about two weeks before the onset of right nasal obstruction causing
extraction of first premolar and molar teeth of right upper jaw due to severe
pain without prominent pain relief. Concomitant with complete right nasal
obstruction he noticed non-tender stiff bulging of right hard palate. Also, the
patient complained of ipsilateral anosmia epiphora and intermittent epistaxis.
Patient’s
past medical history showed chronic rhinosinusitis and he had a surgical
history of septoplasty about twelve years ago. There was no history of
addiction to tobacco or other drugs.
On
examination right sided facial tenderness was detected and oral examination
showed a non-tender compressible mass located on the right side of hard palate
which was exceeded from the midline (Figure 1).

Figure
1.
Extension of the mass into oral cavity presented as right hard palate bulging.
Anterior
rhinoscopy and rigid nasopharyngoscopy revealed a fleshy, greyish pink polypoid
mass that bled easily with minimal manipulation.
No
enlarged cervical lymph nodes were palpated.
Computed
tomography (CT) scan showed a right maxillary sinus soft-tissue density mass
which was destructive in nature with maximal length of about seven centimeters
occupying the whole right maxillary sinus and ipsilateral nasal cavity
extending to oral cavity with bony destruction of medial maxillary sinus wall,
right nasal turbinates, nasal septum and right hard palate but sparing orbital
floor.
Magnetic
resonance imaging (MRI) with and without gadolinium demonstrated a T1
hypointensity and T2 hyperintensity with a bright mass on T1
with contrast within right maxillary sinus and nasal cavity extending to
ethmoid cells superiorly and oral cavity inferiorly (Figure 4b).
Histopathological
examination with immunohistochemistry (IHC) study showed bundles of spindle
cells proliferation with atypia and positive for SMA, CD31, BCL2
and EMA with hemangiopericytoma- like pattern suggestive of glomangiopericytoma
(Figure 2).
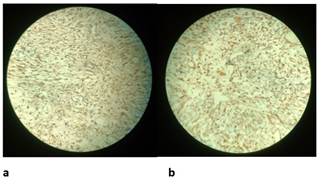
Figure
2.
Muscle actin (SMA) as seen above (a) and B cell lymphoma 2 (BCL2)
markers (b).
The
patient underwent a right open subtotal maxillectomy approach with
Weber-Ferguson incision and the tumor was resected completely (Figure 3) with
safe margins and for better local control, bony boundaries invaded by the tumor
were drilled too.
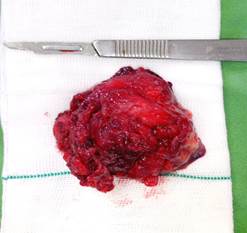
Figure
3. A
spongy compressible mass was resected completely from right maxilla and nasal
cavity with maximal diameter of 7 cm.
Finally,
a full-thickness skin graft was harvested from anterolateral part of right
thigh and transplanted to the posterosuperior and anterior walls of the space
helping better mucosalization of the cavity.
Also,
a hard palate obturator prosthesis was used to close the palatal defect.
The
operation was followed by intensity-modulated radiation therapy (IMRT) over
right maxilla in 30 fractions and for a total of 65 Gy. Our patient remained
free of local or regional recurrence after one year post operation as followed
by regular visits and CT scans (Figure 4a).
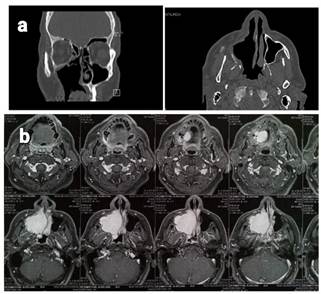
Figure
4. Coronal and
axial view of paranasal sinuses CT scan one year post operation, No evidence of
recurrence is seen (a). Axial T1 with gadolinium injection
before surgery demonstrates a bright mass (b).
Discussion
Glomangiopericytoma
is a kind of hemangiopericytoma found in head and neck especially sinonasal
tract originating from pericytes attached on the surface of capillaries acting
as sphincters with the function of blood flow control (9).
Hemangiopericytoma
is considered a rare soft tissue tumor usually (85%) found in retroperitoneum
and lower extremities and less common (15%) in head and neck region which is
known as glomangiopericytoma (9, 10). Most common sites of involvement in head
and neck are scalp, face, neck, nasal cavities and paranasal sinuses (11).
Nasal cavities are twice more involved and between paranasal sinuses,
involvement of ethmoid cells and sphenoid sinuses with glomangiopericytoma is
about four times more often seen than it does in maxillary sinuses (12). In our
case we could not determine the exact origin of tumor as the whole right
sinonasal cavity was involved by the tumor.
Gender
distribution is almost equal although some studies report a slight female
dominancy (6) contrary to our case who was a man. It is commonly seen in the
sixth and seventh decades of life and more than 80% of patients are Caucasian
(3, 7) but our patient was just 48 years old and the tumor appeared at least
one decade earlier. However, the exact
etiology is unknown but some risk factors including trauma, hypertension, long
term steroid use and pregnancy have been suggested as predisposing factors (3,
6, 7, 12). The patient we reported here had none of the risk factors.
Glomangiopericytoma
is considered as a painless very slow growing mass and hence found in large
sizes when medical diagnosis is made (13). Nasal obstruction is the most common
presentation (60%) followed by intermittent epistaxis (50%), pain, proptosis
and epiphora (11). Our patient’s chief complaint was unilateral nasal
obstruction and facial pain. On rigid endoscopy glomangiopericytoma is appeared
as a soft, fleshy, and red to greyish pink mass which is edematous to
hemorrhagic and easily bleeds (14). There is no relationship between tumor
behavior and anatomical site in the literature but generally about 10% of the
cases will finally encounter distant metastasis through hematogenous route and
usually to lungs, bones and liver and up to 40% will have local recurrence (4,
11).
As
biopsy is not recommended due to severe bleeding, complete radiological
examination by CT and MRI should be performed. A CT scan shows a soft tissue
mass which possible bone destruction is clearly demonstrated and in case of
contrast administration strong enhancement is seen (6, 15). Because of poor
ability of CT scan to differentiate between mass and inflammatory fluid MRI is
mandatory as well (6). On T1 weighted MRI, glomangiopericytoma
appears as a solid hypointense to isointense mass with bright enhancement after
intravenous contrast injection and on T2 weighted imaging, contrary
to inflammatory fluid, glomangiopericytoma appears as a moderate to low
intensity mass (14). The patient had preoperative CT imaging which consistently
demonstrated non-specific findings of mass-like lesion of the para-nasal sinuses
extending up toward the skull base. MRI with contrast administration and
in-office endoscopy showed a vascular and easily bled mass.
Estimating
the risk of clinical aggressiveness is very hard and although a certain
potential of malignancy should always be taken into account, several malignancy
criteria have been established including histological necrosis, nuclear atypia,
high number of mitosis and a large tumor size of >6.5 cm (5, 9).
Diagnosis
of glomangiopericytoma is based on histopathology. Hematoxylin and eosin
staining reveals many vascular vessels and perivascular hyalinization with
uniform oval shaped cells and round to spindle shaped nuclei but it is
immunohistochemistry studies that can differentiate soft tissue
hemangiopericytoma from sinonasal hemangiopericytoma by characteristic reaction
for actin and vimentin (1, 2, 4). Immunohistochemistry evaluation in our
patient was consistent with positive muscle actin (SMA) and B cell lymphoma 2
(BCL2) markers which are charecteristic for GPC.
The
treatment of choice is wide local excision which is done in two main endoscopic
and open approaches. Considering the fact that completeness of resection is
known as the main predictor of recurrence, the literature advices endoscopic
resection to be kept for those tumors with small size, definitely identified
site of origin and tumors undergone preoperative embolization with Onyx
although patient’s preference and surgeon’s technical expertise should be
considered when final decision is to be taken (6, 9). Due to large size of our
patient’s mass and inability to determine the origin of the mass by endoscopic
approach he went under an open surgical approach. Radiotherapy as a primary
treatment modality has a recurrence rate as high as 50% but when used as an
adjuvant therapy in case of incomplete resection of the tumor it had a
statistically lower rate of recurrence but no difference in overall survival
rate (1, 6, 9, 11, 13). Although there are some chemotherapy agents used as
trial studies, currently there is no evidence for or against the use of
chemotherapy agents in hemangiopericytoma or hemangiopericytoma-like tumors
including glomangiopericytoma (1, 6, 11, 16-18). Our patient received
appropriate adjuvant radiotherapy and he was free of tumor residue or
recurrence up to one year of follow-up.
Conclusion
Sinonasal
hemangiopericytoma or glomangiopericytoma is considered as a rare sinonasal
tumor and differs from usual somatic hemangiopericytoma in the anatomical site
of tumor origin, biological behavior and histopathological properties. It is
classified as a low-grade borderline malignancy tumor and should be considered
when imaging and endoscopic evaluations show a soft tissue polypoid vascular
nasal cavity mass. Complete excision of the tumor is the treatment of choice.
Due to the high rate of recurrence even 17 years after the initial
presentation, long-term follow-up is required (Table 1).
Table
1. Glomangiopericytoma
(summarized).
|
Clinical features |
Risk factors |
Imaging findings |
IHC findings |
Treatment |
|
Unilateral
nasal obstruction |
Pregnancy |
Soft tissue
mass in CT scan |
SMA + |
Wide complete
resection ± radiotherapy |
|
Epistaxis |
Trauma |
Bright signal in MRI |
BCL2+ |
|
|
Headache or
facial pain |
Long term steroid |
|
|
|
Future
research
Future
studies are needed to clarify the most important risk factors and the exact
pathogenesis and also to standardize the criteria for adopting the best
surgical approach (endoscopic or open) and post-operative follow-up.
Author
contribution
EA and AT
contributed to data gathering involved in drafting the manuscript, EA
drafted the initial manuscript and AT provided a review of the
manuscript. Both authors approve of the final manuscript.
Conflict
of interest
The
authors declare that they have no conflict of interest.
Funding
The
publishing of this article was supported by student research committee,
Baqiyatallah University of Medical Sciences, Tehran, Iran.
References
1.
Asimakopoulos P, Syed MI, Andrews T, Syed S, Williams A. Sinonasal
glomangiopericytoma: Is anything new? Ear Nose Throat J. 2016; 95 (2): E1-5.
2.
Verim A, Kalaycik Ertugay C, Karaca CT, Gunes P, Sheidaei S, Oysu C. A rare
tumor of nasal cavity: glomangiopericytoma. Case Rep Otolaryngol. 2014; 2014:
282958.
3.
Nichol AA, Bernard BJ, Gilani S. A case report of sinonasal
glomangiopericytoma: An important reminder to always collect specimen. Sci
Prog. 2024; 107(2): 368504241253679.
4.
Dandekar M, McHugh JB. Sinonasal glomangiopericytoma: case report with emphasis
on the differential diagnosis. Arch Pathol Lab Med. 2010; 134 (10): 1444-9.
5.
Stout AP, Murray MR. Hemangiopericytoma: a vascular tumor featuring
Zimmermann’s pericytes. Ann Surg. 1942; 116: 26–33.
6.
Ledderose GJ, Gellrich D, Holtmannspotter M, Leunig A. Endoscopic Resection of
Sinonasal Hemangiopericytoma following Preoperative Embolisation: A Case Report
and Literature Review. Case Rep Otolaryngol. 2013; 2013: 796713.
7.
Schauwecker N, Davis S, Perez A, Labby A, Mannion K, Sinard R, et al. Single
Institution Experience With Sinonasal Glomangiopericytoma: A Case Series. Ear
Nose Throat J. 2023; 17: 1455613231179688.
8.
Al Saad S, Al Hadlaq R, Al-Zaher N. Glomangiopericytoma (Hemangiopericytoma) of
the maxillary sinus and sinonasal tract. Hematol Oncol Stem Cell Ther. 2017; 10
(2): 96-8.
9.
Millman B, Brett D, Vrabec DP. Sinonasal hemangiopericytoma. Ear Nose Throat J.
1994; 73 (9): 680-7.
10.
Gengler C, Guillou L. Solitary fibrous tumour and haemangiopericytoma:
evolution of a concept. Histopathology 2006; 48 (1): 63-74.
11.
Duval M, Hwang E, Kilty SJ. Systematic review of treatment and prognosis of
sinonasal hemangiopericytoma. Head Neck. 2013; 35 (8): 1205-10.
12.
Palacios E, Restrepo S, Mastrogiovanni L, Lorusso GD, Rojas R. Sinonasal
hemangiopericytomas: clinicopathologic and imaging findings. Ear Nose Throat J.
2005; 84 (2): 99-102.
13.
Ceylan A, Degerliyurt K, Celenk F, Atac MS, Sabri Uslu S. Haemangiopericytoma
of the hard palate. Dentomaxillofac Radiol. 2008; 37 (1): 58-61.
14.
Gillman G, Pavlovich JB. Sinonasal hemangiopericytoma. Otolaryngol Head Neck
Surg. 2004; 131 (6): 1012-3.
15.
Chihani M, Aljalil A, Touati M, Zoubeir Y, Labraimi A, Ammar H, et al.
Glomangiopericytoma: An uncommon sinonasal perivascular tumor with particular
characteristics. Egypt J Ear Nose Throat Allied Sci. 2011; 12 (3): 167-70.
16.
Michi Y, Suzuki M, Kurohara K, Harada K. A case of hemangiopericytoma of the
soft palate with articulate disorder and dysphagia. Int J Oral Sci. 2013; 5
(2): 111-14.
17.
Maresi E, Tortorici S, Campione M, Buzzanca ML, Burruano F, Mastrangelo F, et
al. Hemangiopericytoma of the oral cavity after a ten-year follow-up. Ann Clin
Lab Sci. 2007; 37 (3): 274-9.
18. Allah Abu Rass NA, Surougi ER, Baheydarah
ShM, Baroom AH, ALGhamdi H, et al. Neoplasms of the palate: a review. Egypt J
Hosp Med. 2018; 70 (8): 1393-1400.