Fiber-optic bronchoscopy for diagnosing
hilar masses of the lung: a study from a tertiary care cardiothoracic and
vascular centre in northeastern India
James Thiek 1 *, Mrinmoy Talukdar 1, Akash
Guha 2
1 Department of CTVS, Guwahati Medical College and Hospital ASSAM,
India
2 Department of Surgical Oncology, BBCI, ASSAM, India
Corresponding
Authors: James Thiek
* Email: jmsthiek@gmail.com
Abstract
Introduction: Fiberoptic Bronchoscopy is an important tool at a clinician's disposal for
managing various pulmonary pathologies both benign and malignant. Its
sensitivity and specificity highly depend on the site of the pulmonary lesion
with central lesions providing better results than peripheral ones. The
procedure is usually well tolerated if done properly with most complications
being amendable to conservative management. Specially for hilar masses of the
lung bronchoscopy not only allows for obtaining biopsy tissue but also
evaluation of the anatomy for operative planning.
Materials and methods: Herein we review the findings and complications of Bronchoscopy
done for Hilar masses at our institute from 01/05/23 to 01/12/23. In our
study we included patients who had hilar lung masses on imaging and patients
who did not have prior biopsy/FNAC. Patients with peripheral lung lesions and
patients who had a performance status of Eastern Cooperative Oncology Group
more than 2 were excluded from the study.
Results: The results for the 20 cases taken up for bronchoscopy were as follows:
A definite lesion could be identified for biopsy in 14 cases, and samples
biopsied and sent for HPE (Histopathological evaluation) and IHC
(immunohistochemistry) were mostly adequate. The sensitivity of bronchoscopy
was found to be 70%. The procedure was well tolerated and of the total number
of patients taken up for bronchoscopic biopsy only
two patients had complications and these complications were managed
conservatively without the need for further procedure.
Conclusion: In this study bronchoscopy and biopsy were found to be a safe and
effective tool in the management of hilar masses of lung. The study is not
without limitations though which include the short study duration, limited
sample size, and absence of bronchoscopic ultrasound
technology at our institute.
Keywords: CTVS, Cancer, Lung cancer
Introduction
With
the advent of the the first bronchoscopy which was
performed in 1887 by Gustav Killian of Freiburg, Germany the scope and
techniques of the procedure have come a long way from then (1). Fiberoptic
Bronchoscopy is quite frequently being used in the diagnosis of various pulmonary
pathologies including lung cancer. The diagnostic yield of bronchoscopy highly
depends on the site of the lesion with better results for central than
peripheral.
Central
tumours can present as exophytic mass lesions, as peribronchialtumours or with submucosal infiltration of the
bronchial tree. The changes in case of peribronchialtumours
or tumors with submucosal infiltration are subtle and may present with features
such as erythema, loss of bronchial markings and nodularity of the mucosal
surface. Central lesions are usually sampled with a combination of bronchial
washes, bronchial brushings and endobronchial biopsies. The yield of
endobronchial biopsies is highest for exophytic lesions, with a diagnostic
yield of ∼90% (2-4).
Peripheral
lesions are usually sampled with a combination of bronchial wash, brushes,
transbronchial biopsy and TBNA. The diagnostic yield of bronchoscopy for
peripheral lesions depends lesion size, the distance of the lesion from the
hilum and on the relationship between the lesion and bronchus. The yield of
bronchoscopy for lesions <3 cm varies from 14–50% compared with a diagnostic
yield of 46–80% when the lesion is >3 cm (5-7).
As
observed in the study by Stahl etal the mechanical
complications of bronchoscopy are primarily related to airway manipulations or
bleeding while the systemic complications arise from the procedure itself,
medication administered, or patient comorbidities; but still mortality rates
remain low at < 0.1%. Thus fiber-optic bronchoscopy offers an effective
and safe diagnostic modality for hilar mass of the lung, with good diagnostic
yield and low mortality rate (8).
Histopathological
Evaluation with Immunohistochemistry and location of the tumor with respect to
the hilum is of utmost importance when planning treatment modality when it
comes to carcinoma of lung. Bronchoscopy can help provide both. Thus bronchoscopy is routinely done at out centre for hilar masses of lung and thus this retrospective
study was done to evaluate its efficacy and safety.
Material and methods
In this retrospective study we review the findings
and post procedure complications of Bronchoscopy done for Hilar masses in a
dedicated Oncology centre from 01/05/23 to 01/12/23.
It is a retrospective study where data was collected
from records.The total
number of cases included in the study from 01/05/23 to 01/12/23 is 20.
Inclusion criteria
1)
Patients
who had hilar lung masses on imaging were included in the study.
2)
Patients
who did not have prior biopsy/FNAC done were included in the study.
Exclusion criteria
1)
Patients
with peripheral lung lesions were excluded from the study.
2)
Patients
who had a performance status of Eastern Cooperative Oncology Group more than 2
were excluded from the study.
The main aim of the study was to review fiber-optic
bronchoscopy as a safe and effective tool for diagnosis and evaluation of hilar
mass of the lung.
Results
Age distribution
In our study, nine of the patients were aged 50 to
59, nine were between 60 and 69, and only two were above 70. The mean age of
the patients was 61.25 (Table 1 and Figure 1).
Table 1. Showing the age distribution of the
patients presenting with hilar mass of the lung.
|
Age distribution |
Number of patients |
|
<50 |
0 |
|
50- 59 |
9 |
|
60- 69 |
9 |
|
>70 |
2 |
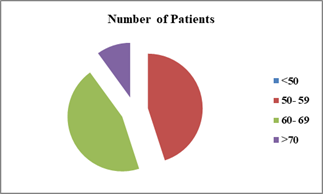
Figure 1. Showing the age
distribution of the patients presenting with hilar mass of the lung.
Sex
distribution
Sixteen of the patients were male and four were
female resulting in the M:F ratio of 4:1 (Table 2 and Figure 2).
Table 2. Showing the sex distribution in the
patients taken up for the study.
|
Sex Distribution |
Number of patients |
|
Male |
16 |
|
Female |
4 |
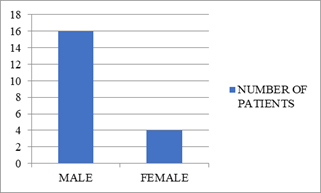
Figure 2. Showing the sex distribution in the patients taken up for the study.
Site
of lesion
In
our study 14 patients (70%) had right sided lesions and 6 patients(30%)
had left sided lesions (Table 3 and Figure 3 and Figure 4).
Table 3. Showing the side of the hilar mass in
the study patients.
|
Site |
Number of patients |
|
Right hilar mass |
14 |
|
Left hilar mass |
6 |
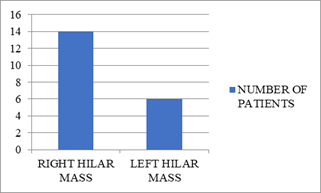
Figure 3. Showing the side of the hilar mass in the
study patients.
A

B

C

D
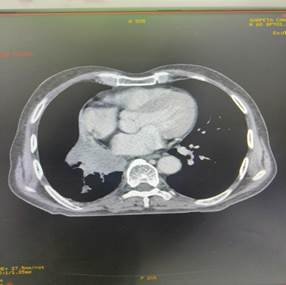
Figure 4. A,B,C, and D
show the right hilar mass on contrast-enhanced computerized tomography thorax.
Final
histopathology
Ten
of the biopsy specimens showed squamous cell carcinoma, one showed
adenocarcinoma and three showed poorly differentiated carcinoma or other
cellular variants. In six of the patients no endobronchial lesion could be seen
for biopsy (Table 4 and Figures 5 and 6).
Table 4. Showing the final histopathology of the
biopsy specimen obtained during the study.
|
Histopathology |
Number of patients |
|
Squamous cell carcinoma |
10 |
|
Adeno carcinoma |
1 |
|
Poorly differentiated carcinoma/others |
3 |
|
|
|

Figure 5. Showing the final histopathology of the
biopsy specimen obtained during the study.
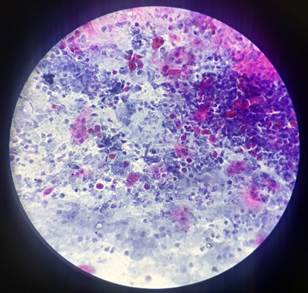
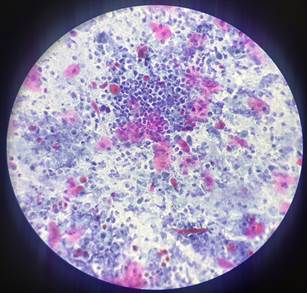
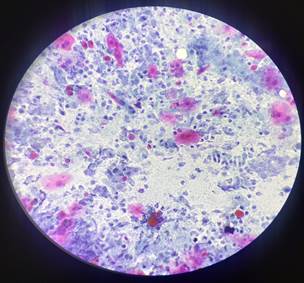
A
B
C
D
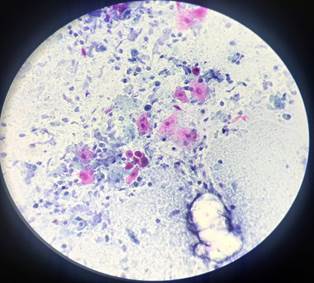
Figure 6. A, B, C and D show bronchoalveolar lavage
cytology with the presence of malignant cells.
Lesion
on bronchoscopy
14 of the cases showed a definitive lesion, and in
all of these instances, a biopsy was taken. Thus, the sensitivity of
bronchoscopy was found to be 70 percent (True positive/true positive + false
negative) (Table 5 and Figures 7 and 8).
Table 5. Showing the total number of cases
wherein definite lesion could be seen on bronchoscopy.
|
Lesion on bronchoscopy |
Number of patients |
|
Seen |
14 |
|
Not seen |
6 |
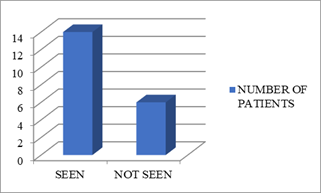
Figure 7. Showing the total number of cases
wherein definite lesion could be seen on bronchoscopy.
A
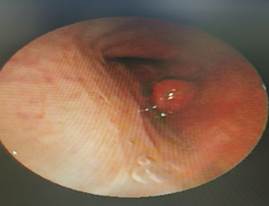
B

C

D

Figure 8. A, B, C and D show growth encountered
during bronchoscopy.
Complications
Only
two of the patients developed intra procedure complications a) haemorrharage from biopsy site and b) transient respiratory
distress both of which were managed conservatively (Table 6 and Figure 9).
Table 6. shows the complication spectrum post
procedure.
|
Complications |
Number of cases |
|
Haemmohorage |
1 |
|
Respiratory
distress |
1 |
|
Bronchospasm |
0 |
|
Pneumothorax |
0 |
|
Respiratory
Failure |
0 |
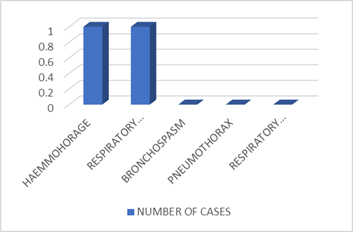
Figure 9. Showing the complication spectrum post procedure.
Discussion
As
per Dela Cruz etal 0.2% of lung cancer was diagnosed in patients between
age 20 and 34 years; 1.5% between 35 and 44 years; 8.8% between 45 and 54
years; 20.9% between 55 and 64 years; 31.1% between 65 and 74 years; 29%
between 75 and 84 years; and 8.3% at 85 years and older, which showed similar
trend with our study with 45% patients in the age bracket of 50-59 years and
45% of the patients in the age bracket of 60-69 and 10% of patients in the
>70 years age bracket (9). The male-to-female ratio was 3.5:1 in the study
by Noronha et al. which was similar to our study at a ratio of 4:1(10). Our
findings were a bit different with regard to the study by Noronha et al which
showed eight percent of patients had small-cell carcinoma; of the 92% patients
with non-small-cell carcinoma (NSCLC), the most common histology was
adenocarcinoma (43.8%), followed by squamous cell (26.2%), large cell (2.1%)
and other (8.3%), while in our study we found that 50% of patients had squamous
cell carcinoma, 5% had adenocarcinoma and 15% had poorly differentiated
carcinoma while definite histopathological diagnosis could not be made in 30%
of the cases This discrepancy may have arisen due to the high incidence of
tobacco smoking in this region. As for the high rate of absence of
histopathological diagnosis, it may be due to the absence of transbronchal ultrasonography guided fine needle aspiration
cytology along with high prevalence of pulmonary tuberculosis in this region
which can mimic lung lesions. For the cases taken up for bronchoscopy a
definite lesion could be identified for biopsy in 14 cases which accounts for
70% accuracy which is similar to the findings by acharya et al who found bronchoscopic procedures had a high diagnostic accuracy of
81.25% in confirming lung malignancies in central tumours
(11). The samples biopsied and sent for HPE(Histo-pathological evaluation) and IHC(Immuno-histo chemistry) were mostly adequate. The procedure was
well tolerated and of the total number of patients taken up for bronchoscopic biopsy only two patients had complications
one of whom had minor bleeding and the other had respiratory distress which is
similar to the findings by M. Modoni et al who
found the most frequent complication in
their study to be minor bleeding, which can resolve spontaneously in the
majority of the cases or can be treated with ice-cold saline or
vasoconstrictive agents (12). The complications encountered in our study were managed
conservatively without the need for ICU care or other invasive/surgical
modalities.
Conclusion
On
reviewing the findings of this retrospective study it
was observed that bronchoscopy and biopsy is a safe and effective tool which
provides anatomical picture along with tissue for HPE and IHC in case of lung
lesions presenting with hilar masses on imaging. The main limitations of the
study include the short study duration, small sample size,.
and absence of endoscopic ultrasonography.
Author
contribution
JT study design and data collection and compiling, AG, pictures and
tables, MT supervisor. All authors reviewed the manuscript.
Conflict
of interest
There
is no Conflicts of interest/competing interests.
Funding
There
is no funding.
Ethical
approval
The
paper was put before the ethical board but as it was a retrospective study and
as the bronchoscopy is a routine investigation done at our centre
for lung masses as per our institute protocol it was decided by the board that
ethical clearance would not be needed for the study.
Consent
Informed
and written consent was taken for all cases included in the study.
References
1.
KilIian G. UeberdirecteBronchoscopie. MMW 1898; 27: 844–847.
2.
Wilson RW, Frazier AA. Pathological-radiological
correlations: pathological and radiological correlation of endobronchial
neoplasms: part II, malignant tumors. Ann DiagnPathol 1998; 2: 31–34.
3.
Simoff MJ. Endobronchial
management of advanced lung cancer. Cancer
Control 2001; 8: 337–343.
4.
Schreiber G, McCrory DC. Performance
characteristics of different modalities for diagnosis of suspected lung cancer:
summary of published evidence. Chest 2003; 123: 115S–128S.
5.
Gasparini S. Bronchoscopic biopsy techniques in the diagnosis and
staging of lung cancer. Monaldi Arch Chest
Dis 1997; 4: 392–398.
6.
Hanson RR, Zavala DC, Rhodes ML, et
al. Transbronchial biopsy via flexible fiberoptic bronchoscope: Result in
164 patients. Am Rev Respir Dis 1976; 114: 67–72.
7.
Govert JA, Dodd LG, Kussin PS, et al. A prospective comparison
of fiberoptictransbronchial needle aspiration and
bronchial biopsy for bronehoscopically visible lung
carcinoma. Cancer 1999; 87: 129–134.
8.
Stahl DL, Richard KM, Papadimos TJ. Complications of bronchoscopy: A concise
synopsis. Int J CritIllnInj Sci. 2015
Jul-Sep;5(3):189-95.
9.
Dela Cruz CS, Tanoue LT, Matthay RA. Lung cancer: epidemiology, etiology, and
prevention. Clin Chest Med. 2011 Dec;32(4):605-44.
10.
Noronha V, Dikshit R, Raut N, Joshi
A, Pramesh C S, George K, Agarwal J P, Munshi A, Prabhash
K. Epidemiology of lung cancer in India: Focus on the differences between
non-smokers and smokers: A single-centre experience.
Indian J Cancer 2012;49:74-81
11.
Acharya K V, B U, Shenoy A, Holla R.
Utility of Various Bronchoscopic Modalities in Lung
Cancer Diagnosis. Asian Pac J Cancer Prev. 2017 Jul 27;18(7):1931-1936.
12.
Mondoni M, Rinaldo RF,
Carlucci P, Terraneo S, Saderi
L, Centanni S, et al. Bronchoscopic sampling
techniques in the era of technological bronchoscopy. Pulmonology.
2022;28(6):461–71.