Effect of inter-personal
communication on cervical cancer knowledge and prevention among women in Rural
Bengaluru, India
Garima Kumari
1, H R Raveendra Reddy 2, Nivedita B M 2 *
1 Novo Nordisk, Bengaluru, Karnataka, India
2 Department of Community Medicine, Vydehi Institute of Medical
Science and Research Centre, Bengaluru, Karnataka, India
Corresponding
Authors: Nivedita B M
* Email: drritudesai@gmail.com
Abstract
Introduction: Cervical cancer is one of the leading causes of
cancer among women worldwide. In 2012, 528,000 new cases of cervical cancer
were diagnosed globally, 85% of which were in less developed countries of
Sub-Saharan Africa, Asia (including India) and Central and South American
countries. Currently, cervical cancer is the 2nd leading cause
of cancer deaths in India which approximately accounts to 1/3rd of
the global cervical cancer deaths. High-risk types are HPV16 & 18 and they
account for more than 90% of cervical carcinoma and the route of transmission
is mainly by sexual contact, which can be prevented by health education. The
present study was conducted among rural reproductive women where the prevalence
of cervical cancer is high and can be prevented by using a simple intervention
method of health education.
Materials and Methods: An interventional, community-based comparative study was conducted
among 388 women of reproductive age residing in Whitefield, Bengaluru, over a
period of one and a half years (May 2016 – October 2017). The pre-tested,
semi-structured (Questionnaire) data collection tool was used to collect data
before and after intervention (IPC).
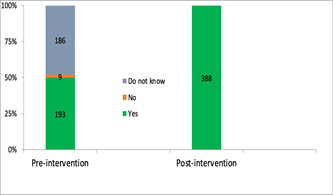
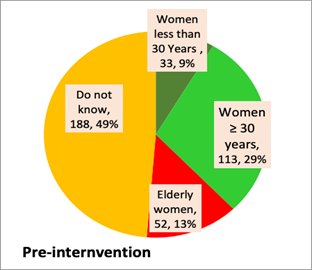
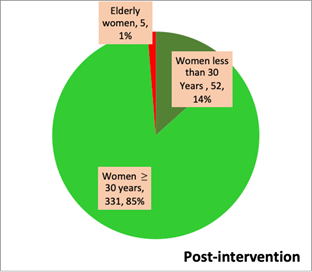
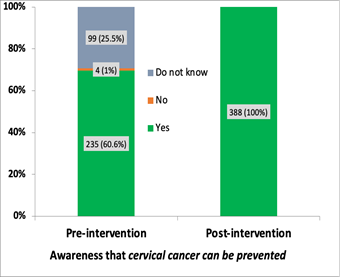
Results: Out of 388 women who participated in the study, the majority 223
(57.48%) belonged to the age group of 15-29 years. The awareness about cervical
cancer significantly improved post-intervention (IPC). 26.29% had underdone pap
smear examination for cervical cancer post-intervention compared to only 18.04%
pre-intervention. The findings suggest a significant improvement in awareness
and screening practices post-intervention.
Conclusion: The findings of the study suggest that there was a positive impact of
Interpersonal Communication on the overall increase in knowledge regarding
Cervical cancer and its prevention among the women of reproductive age group in
the study.
Keywords: Cervical cancer, Knowledge, Inter personnel communication, Prevention
Introduction
Cervical cancer is one of the leading cause of cancer
among women worldwide. In 2012, 528,000 new cases of cervical cancer were
diagnosed globally, 85% of which were in less developed countries of
Sub-Saharan Africa, Asia (including India) and some in Central and South
American countries. And among them 266,000 women died of cervical cancer, and
this was seen more in low and middle income countries.1 According to
World health organisation (WHO), Human papilloma virus (HPV) infection affects
about 10-20% of people between 15-49 years, and out of them 40% are women under
25 years of age.2 Currently, cervical cancer is the 2nd
leading cause of cancer deaths in India which approximately accounts to 1/3rd
of the global cervical cancer deaths.3
Aetiology of cervical cancer is exposure to infection
by Human Papilloma Virus (HPV). There are over 100 types of HPV. Among them
high risk types are HPV-16-18 and it accounts for more than 90% of cervical
carcinoma. Route of transmission of HPV is by sexual contact.4 The
predisposing factors for HPV infection are early age at intercourse, multiple
sexual partners, Other factors like tobacco use and Immuno-suppression (for
example HIV infection) facilitate HPV infection leading to metaplastic change
and which in turn develop into cancer.5 Primary prevention of
cervical cancer aims at decreasing the incidence of cervical cancer by reducing
causes and risk factors. Vaccines against HPV have been developed and proved to
be effective against HPV infection.
The present study was conducted among rural
reproductive women where prevalence of cervical cancer is high due to lack of
knowledge and high risk practices. This can be prevented by using simple
non-invasive method of intervention of health education specifically
inter-personal communication (IPC). This method is chosen on ethical grounds as
the subject is sensitive and taboo associated with female reproductive health,
hence participants wants it to be confidential.
Objectives
•
To determine the knowledge, attitude and practice about the cervical
cancer among women of reproductive age group.
•
To evaluate the impact of Interpersonal Personal Communication and
Counselling on the knowledge, attitude and practices regarding cervical cancer
prevention among women of reproductive age
Materials and methods
Study design: Interventional Community based
comparative study
Study area: The study was carried out in Whitefield
area, situated in the eastern part of Bengaluru city, Karnataka State.
Study period: The study was carried out over a period
of one year and six months (May 2016 – October, 2017)
Study Population: This study was carried out among the
women of reproductive age-group (15- 45 years) residing in study area.
Inclusion Criteria
•
Women aged 15-45 years and residing in the study area for more than 6
months
•
Women who have given consent to participate in the study
Exclusion Criteria
•
Women who had been diagnosed with cervical pre-cancer or cervical cancer
•
Women who had received treatment for cervical pre-cancer or cancer.
Sample size
Assuming that about 44.5% of the study population will
know about cervical cancer (based on a study done by Siddhartha J et al among
women attending a tertiary care hospital in Puducherry), 8 with an absolute
precision of 5%, and 95% Confidence Interval, the sample size was calculated.
Minimum sample size required = 380.
Assuming about 5% of participants may drop out post-
IPC for follow- up interview, a sample size of 400 (380 + 5% of 380) was
considered for the study.
Sampling Technique
Line list of all the houses in the study area having
at least one woman in the reproductive age group (15-45 years) was prepared.
The houses were randomly selected by simple random technique using MS Excel.
House visits were made to each of the selected houses. Details about the study
and confidentially was explained to the eligible study subjects. Women who
fulfilled the inclusion criteria, agreed to participate in the study and gave
written informed consent were included in the study. This method was followed
till the required sample size was reached.
Data collection
Data was collected using semi-structured, pre-tested
questionnaire as data collection tool. The tool was validated by faculty from
the Departments of Community Medicine, Obstetrics & Gynaecology and
Oncology, VIMS and RC. Validated tool was field tested by pilot study with 25
women of reproductive age- group (15-45 years), randomly selected from the
study area. The final tool, after incorporating inputs received during the
pilot testing was used in the study.
The data collection tool had the following parts:
Part I: related to demographic data
Part II: to assess the knowledge, attitude and
practice regarding cervical Cancer.
Data analysis
Data was entered in the data forms created in Epi
InfoTM software Version 7.2.0.1, Centre for Disease Control and Prevention
(CDC), Atlanta and analysed using the same software. The analysed
socio-demographic data is expressed in proportions and percentages. The results
of pre-intervention and post-intervention data were analysed using Mac Nemar’s
test and level of significance by ‘p’ value. The ‘p’ value < 0.05 is
considered to be statistically significant.
Ethical Considerations
The ethical approval for the study was obtained from
Vydehi Institutional Ethics Committee, Vydehi Institute of Medical Sciences and
Research Centre. Written informed consent was obtained from the study
participants and parental consent was obtained for the participants below 18
years. Confidentiality of the data collected was maintained. The anonymity of
the study participants was maintained throughout the study period.
Results
The line list of houses in the study area had 5500
houses, fulfilling the inclusion criteria. From these 5500 houses, 445 women
who were eligible for the study were randomly selected and requested to
participate in the study. Of them 400 women agreed to participate and gave the
consent. Of those 400 women who participated in the study during baseline data
collection, 12 were not available during post intervention data collection.
Hence, the data of 388 (400-12) women who were available during both pre and post
intervention was analysed and the results of the same is presented in this
section.
The results of the study are presented under following
sections:
1. Description of the study subjects
2. Comparison of Knowledge regarding Cervical
Cancer and its prevention before and after the intervention
Table 1. shows most of the study participants (90 out
of 388) are between 20-24 years accounting for 23% followed by 25-29 years
(20%). 45.36% (176 out of 388) are professional and 30% are employed. Majority
of them are married accounting 52.58% whereas 41.24% are single. Most of them
belong to Upper Middle class (Mod. B G Prasad Classification) of Socio-economic
status.
Table 1. Distribution of study subjects based on their demographic profile.
|
Age group |
Number |
Percentage |
|
15-19
years |
53 |
13.66 |
|
20-24
years |
90 |
23.20 |
|
25-29
years |
80 |
20.62 |
|
30-34
years |
73 |
18.80 |
|
35-39
years |
46 |
11.86 |
|
≥ 40 years |
46 |
11.86 |
|
Total |
388 |
100 |
|
Educational
status |
||
|
Professional/Postgraduate |
176 |
45.36 |
|
Graduation |
87 |
22.42 |
|
PUC /12th
grade |
31 |
7.99 |
|
High
School |
39 |
10.05 |
|
Middle
School |
27 |
6.96 |
|
Primary
School |
11 |
2.84 |
|
Illiterate |
17 |
4.38 |
|
Total |
388 |
100 |
|
Occupational status |
||
|
Employed |
120 |
30.93 |
|
self-
employed |
109 |
28.09 |
|
Homemakers |
58 |
14.95 |
|
Students |
101 |
26.03 |
|
Total |
388 |
100 |
|
Marital status |
||
|
Married |
204 |
52.58 |
|
Single |
160 |
41.24 |
|
Separated |
16 |
4.12 |
|
Widowed |
5 |
1.29 |
|
Divorced |
3 |
0.77 |
|
Total |
388 |
100 |
|
Socio
economic status |
||
|
Upper |
70 |
18.04 |
|
Upper
Middle |
269 |
69.33 |
|
Lower
Middle |
32 |
8.25 |
|
Upper
Lower |
17 |
4.38 |
|
Lower |
0 |
0.00 |
|
Total |
388 |
100 |
Table 2. shows 336 women out of 388 (87.88%) were
aware about cervical cancer and for most of them, 55.93% the source of
information were family members followed by friends and relatives who accounts
for 40.72%.