Psychometric
evaluation and factor structure of the Persian coping strategies questionnaire
in chronic low back pain patients
Sarvenaz
Karimi-GhasemAbad 1,2 *, Behnam Akhbari 2, Mahyar
Salavati 2, Saeed Talebian Moghaddam 3, Ahmad Saeedi 4,
Mahsa Seydi 5, Mohammad Ali Shakoorianfard 6
1 Razi Hospital, School of Medicine, Guilan University Medical
Sciences, Rasht, Iran
2 Physiotherapy Department of University of Social Welfare and
Rehabilitation Sciences, Tehran, Iran
3 Physiotherapy Department of Tehran University of Medical Sciences,
Tehran, Iran
4 Department of Statistical Research and Information Technology,
Institute for Research and Planning in Higher Education, Tehran, Iran
5 Neuroscience Research Australia of University of New South Wales,
Sydney, Australia
6 Physiotherapy Department of Physiotherapy Department of Iran
University of Medical Sciences, Rehabilitation Faculty, Tehran, Iran
Corresponding
Authors: Sarvenaz Karimi-GhasemAbad
* Email: s_karimi@gums.ac.ir
Abstract
Introduction: This study aimed to investigate the factor
structure and psychometric properties of the Coping Strategies Questionnaire
(CSQ) in Persian in people with non-specific chronic low back pain (NSCLBP).
Materials and methods: Exploratory factor analysis (EFA) and confirmatory factor analysis
(CFA) were employed to determine the CSQ's factor structure. Reliability was
assessed using the Intraclass Coefficient and Cronbach's Alpha.
Results: 13 variables, accounting for 74.94% of the total variance, were
identified using EFA; based on Parallel Analysis, the first four
components—ignoring pain sensations, praying, diverting attention, and
catastrophizing—were kept. A sufficient model fit was not shown by the CFA
results (χ²/df = 1.77, CFI = 0.884, TLI = 0.84, and RMSEA = 0.081). All
subscales had Cronbach's alpha and test-retest reliability between 0.75 and
0.88 and 0.7 and 0.83, respectively.
Conclusion: According to the study's findings, there are four-factor structures in
the Persian version. Additionally, it was stated that the item-total
correlations, agreement, and test-retest reliability were all at a good and
acceptable level.
Keywords: Coping strategies questionnaire, Chronic non-specific low back pain,
Factor structure, Psychometric properties, Parallel analysis
Keywords: Breast cancer, MCF-7, Radiosensitizing, Radiotherapy
Introduction
The term "coping" describes the methods
employed to address the detrimental impacts of stress. These strategies
encompass ways people address pain and disability, and are both cognitive
(e.g., praying, counting numbers, and activities that create a sense of
detachment from the environment) and behavioral (e.g., walking and talking to
others)(1).
The type of coping strategy varies depending on the
situation and culture; thus, an adaptive solution (or maladaptive: Coping strategies, such as catastrophizing, are associated with increased
pain and disability) in a culture may be maladaptive (or adaptive: Coping
strategies, such as ignoring pain, have been associated with reduced pain and
disability) in another (2). In recent years, researchers pay more attention to the importance of the
effects of appraisal and coping on the performance of people with chronic pain,
Studies have also reported a moderate to strong association between coping
strategies, pain intensity, psychological characteristics, and physical
function (3).
Review
articles have established a relationship between maladaptive coping strategies
and persistent pain control challenges in individuals experiencing chronic
lower back pain. Studies have found that coping strategies including praying,
hoping, and diverting attention are more closely associated with the degree of
pain, whereas self-statements and pain-ignoring techniques are better
indicators of disability. However, inconsistent findings in the literature
highlight the complexity of categorizing coping strategies as adaptive or
maladaptive. Pain is experienced and managed differently across cultures,
leading to variability in coping strategies and their effects on pain. The
significance of specific coping strategies is influenced by cultural variables
and the metrics used to evaluate outcomes. In addition, personality traits
themselves may differ across cultures. The impact of coping strategies on
disability resulting from chronic low back pain within Iranian society remains
unclear(4).
One of the appropriate tools for evaluating and
identifying coping strategies is the Coping Strategies Questionnaire (CSQ),
designed by Rosenthal and Keefe in 1983 and frequently used in studies (5). One advantage of this tool is its patient-centered approach, which
assesses patients’ problems across all dimensions, particularly their quality
of life, along with its robust psychometric properties (6). The original version of this scale contains 48 items (5). The questionnaire has been adapted into six
languages, with acceptable validity and reliability; however, no stable factor
structure has been reported (7-13). Asghari et al. (2005) translated this questionnaire into Persian among
people with chronic pain and finally designed a 42-item Persian version. Six
cognitive strategies and one behavioral strategy are included in this
assessment (9). The seven subscales' Cronbach's alpha coefficients varied from 0.74 to
0.83, demonstrating the high level of internal consistency (9). Prior research examining the factor
structure of the CSQ has not identified a consistent and valid factor
configuration, although certain patterns have emerged across various
populations, cultures, and methodologies (14-17).
Researchers
hypothesize that these differences could be caused by the scales that
Rosenstiel and Keefe (1983) proposed (5), their operationalization, and the
variations in coping methods arising from the heterogeneity of pain conditions
and cultural contexts (13).
The purpose of this study was to comprehensively examine
the Coping Strategies Questionnaire (CSQ)'s factor structure and reliability in
Persian, with a focus on people with NSCLBP. The following are the study's
hypotheses:
1.
The CSQ demonstrates statistically significant and acceptable internal
consistency and test-retest reliability.
2.
Each item’s correlation with the relevant subscale, after deducting the
score of that item, is significant.
3.
The factors extracted in the study
are consistent with the factor structure of the original questionnaire.
Methods
Using
a convenience selection technique, 120 patients with chronic low back pain who
visited physiotherapy centers in Tehran between the fall and winter of 2017
were chosen for this cross-sectional study. An informed consent form, certified
by the appropriate ethics committee, was signed by each participant.
Participants were Persian-speaking, literate, and had a
history of NSCLBP (Chronic back pain can initially be classified as inflammatory
disorders (18); however, over
time, the lack of appropriate treatment, along with psychological risk factors
and the adoption of maladaptive coping strategies, can lead to the development
of chronic back pain ), with pain in the area between the 12th rib and the ischial tuberosity
lasting more than three months(19, 20). Exclusion
criteria included a history of spinal stenosis (21), lumbar discopathy and radicular
pain in the lower extremities (22), pregnancy, and a history of
psychological treatment. Sample size considerations vary: to obtain
valid factors, samples should be representative and sufficient in size.
According to Guilford (23), the minimum sample size is 200 people, however, Kline argues this figure
may be exaggerated, noting that samples of 100 with a clear factor structure
are often adequate (24). Another approach is to use the participant-to-item ratio, with 1:3, 1:6,
and 1:10 ratios commonly recommended. This study adopted a 1:3 ratio (25, 26). Hair et al. also consider a sample size of 100 or more sufficient (27). In the present study, the minimum sample size was set at 120 people.
Sixty participants retook the CSQ ten to twelve days later to assess
reliability (28). The tools used in this study were:
CSQ
The purpose of the Coping Strategies Questionnaire (CSQ)
is to determine the coping mechanisms employed by people with chronic pain.
This assessment consists of 48 items, including six diverse cognitive
strategies and two behavioral strategies, the “increasing pain” item was
excluded from the analysis due to its low reliability. The CSQ comprises seven
subscales, each containing six items: praying or hoping (items 14, 15, 18, 22,
28, 36); coping self-statements (items 6, 8, 20, 23, 31, 32); diverting attention
(items 3, 9, 12, 26, 27, 38); reinterpreting pain sensations (items 1, 4, 10,
16, 29, 41); catastrophizing (items 5, 11, 13, 25, 33, 37); ignoring pain
sensations (items 17, 19, 21, 24, 30, 35); and increasing behavioral activities
(items 2, 7, 34, 39, 40, 42). Seven choices are available for each item: 0
means never use, 3 means use occasionally, and 6 means constantly use. Higher
scores on each subscale, which ranges from 0 to 36, indicate a stronger
preference for a particular coping mechanism. With Cronbach's alpha
coefficients for every subscale surpassing 0.70, the Persian version of the CSQ
exhibits great psychometric qualities as well as good internal consistency
comparable to the original version (9).
Visual analog scale (VAS)
The Visual Analog Scale (VAS) is a popular self-report
instrument for gauging the severity of pain. With endpoints marked "no
pain" and "worst imaginable pain," participants rate their level
of pain by placing a mark on a 100-mm line. The VAS has demonstrated strong
psychometric properties, including reliability and validity, and is a standard
tool in pain research (29, 30).
Statistical Analysis
Reproducibility measures the consistency of results
obtained from repeated administration of a test to the same individuals under
stable conditions (31). Test-retest reliability involves administering
the same assessment to the same participants on at least two occasions (28), To assess the relative reliability, a random two-way model with a
95% confidence interval was employed. Values greater than 0.7 were considered
acceptable for both internal consistency (Cronbach's alpha) and correlation
coefficients (ICC) (31, 32). Scores from many test administrations were evaluated for absolute
reliability using standard error of measurement (SEM) (31), utilizing the equation SEM = s √ (1-r)), in where "s" stands
for the standard deviation and "r" for the ICC. Using the formula,
the minimum detectable changes (MDC) were determined ( ) (32, 33).
) (32, 33).
Agreement: A Bland-Altman
plot was used to evaluate agreement between test and retest subscales. The
outcome measure of this method was the mean difference and limitation of
agreement, with a 95% confidence interval (34).
Item-total
correlation (ITC): ITC was analyzed using the Spearman
correlation coefficient, which allowed the correlation between each item and
the related subscale to be displayed following the subtraction of each item's
score. Correlation coefficients greater than 0.4 were deemed appropriate (35).
Factor
structure: EFA is a multivariate statistical method that reveals latent
factors that account for observable data patterns, thus revealing the
underlying relationships between variables. Factor analysis was implemented
through the use of BM SPSS Amos 17 structural equation modeling
software (SPSS Inc., Chicago, IL, USA). Sample adequacy was evaluated using the
Kaiser-Meyer-Olkin (KMO) test (a value greater than 0.77 indicates
sufficiency), and if considerable variance was found, the Bartlett test of sphericity
was performed to establish whether the items were suitable for component
analysis. Items
were only included in the analysis if their factor loading was larger than 0.4;
eigenvalues >1 were regarded as the main factors (13). In a sample
of Iranian people with NSCLBP, the model fit of the Persian version of the CSQ
was assessed using Confirmatory Factor Analysis (CFA) (31). The model's efficacy was assessed
using the model fit indices, Researchers compare goodness-of-fit indices to
predetermined cutoff values (such as CFI >.950) obtained from simulation
tests in order to assess model fit in CFA. Methodologists have warned that
goodness-of-fit cutoffs are only applicable in environments that are comparable
to the simulated scenarios that inspired them. Fixed cutoffs for common GOFs
(i.e., χ2, χ2/df, CFI, TLI, and RMSEA) are nevertheless often utilized in
practical research in spite of these cautions (36). A good model
fit is indicated by values like χ2 / df < 3, Tucker-Lewis Index (TLI) ≥
0.90, Comparative Fit Index (CFI) ≥ 0.90, and Root Mean Square Error of
Approximation (RMSEA) ≤ 0.08 (37).
Parallel
analysis (PA) was also used to obtain the appropriate number of factors, which
was performed using O’Connor syntax in SPSS-17 software. Data simulation based
on real data and the elimination of variables with eigenvalues less than one
form the basis of this approach. The total amount of factors is the deciding
factor when the simulated data's eigenvalue is higher than the real data's
eigenvalue (38, 39).
Results
The participants' average age was 36.36 years, with a
standard deviation of 10.51 years. According to a 100-mm visual analog scale,
the average pain intensity measured during the evaluation was 30.9 mm.
According to demographic data, 70.8% of participants were female and 29.2% were
male. The distribution of educational backgrounds was as follows: 19.1% had a
diploma, 48.4% had a bachelor's degree, and 32.5% had earned a master's or
doctoral degree. Table 1 contains more background data on the individuals involved.
The data distribution across all subscales was non-normal; therefore,
non-parametric methods were employed for statistical analysis.
Table
1. Demographic characteristics
of subjects with NSCLBP (n=120).
|
Range
|
Mean
|
Standard
Deviation
|
|
Age (year)
|
19-68
|
36.36
|
10.51
|
|
BMI
|
16.02-35.32
|
24.86
|
3.72
|
|
VAS (mm)
|
20-70
|
30.9
|
10.9
|
|
Duration (month)
|
3-240
|
27.84
|
37.28
|
BMI;
Body Mass Index, VAS; Visual Analogue Scale
The test-retest reliability results for all subscales
ranged from 0.75 to 0.88, indicating good reliability. Cronbach’s alpha values
were reported between0.7-0.83, indicating good internal consistency of the
subscales. The subscales' ICC, SEM, MDC, and Cronbach's alpha values are
displayed in Table 2.
Table
2.
Test-retest reliability of Persian version of CSQ in subjects with NSCLBP
(n=50).
|
Subscales
|
ICC
(95% interval confidence)
|
Cronbach’s alpha
|
SEM
|
MDC
|
|
Diverting
attention
|
0.74(0.60-0.83)
|
0.79
|
3.48
|
9.64
|
|
Reinterpretation
|
0.85(0.77-0.91)
|
0.77
|
2.63
|
7.29
|
|
Catastrophizing
|
0.85(0.76-0.90)
|
0.83
|
2.77
|
7.67
|
|
Ignoring pain
|
0.78(0.66-0.86)
|
0.83
|
3.42
|
9.47
|
|
Praying/hope
|
0.88
(0.81-0.93)
|
0.82
|
3.21
|
8.89
|
|
self-statement
|
0.78 (0.67-0.86)
|
0.80
|
3.28
|
9.09
|
|
Increasing
activity levels
|
0.82 (0.72-0.89)
|
0.7
|
2.68
|
7.44
|
ICC:
intraclass correlation coefficient, SEM: Standard Error of Measurement, MDC:
minimal detectable
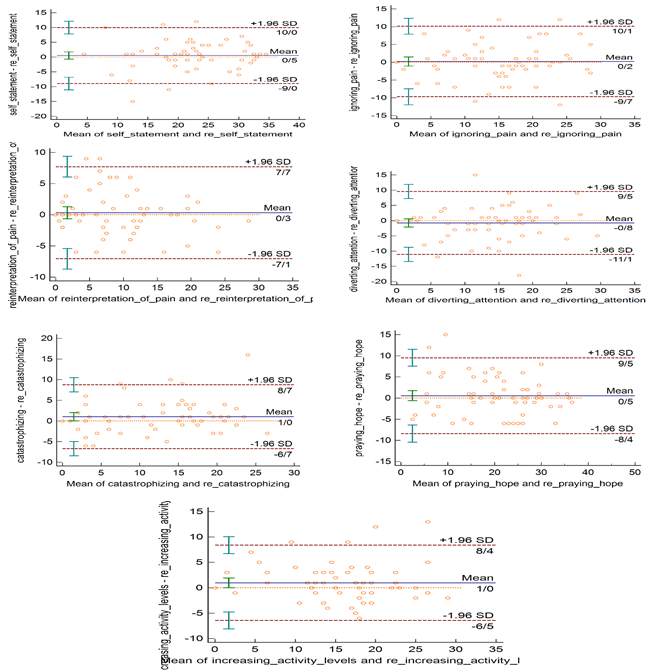
The results of Bland-Altman Plots indicated that the mean
difference of all subscales ranged from -0.8 to 1, with upper and lower limits
of agreement ranging from 7.7 to 10.1 and -11.1 to -6.5, respectively. Figure 1
configured Bland-Altman Plots of all 7 subscales of the CSQ.
The Spearman correlation between each item and its
matching subscale varied from 0.358 to 0.707, as seen in Table 3. According to
this data, each item's correlation with its subscale was consistently higher
than its association with other subscales. Furthermore, all items exhibited a
statistically significant correlation with their respective subscales, with a
P-value of less than 0.001.
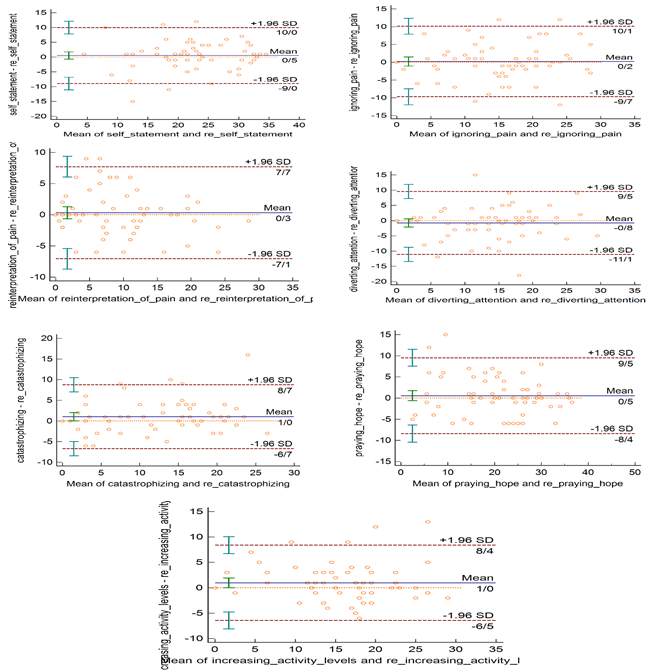
Figure
1. Bland-Altman
Plot of subscales of Coping strategies Questionnaire in subjects nonspecific
chronic Low Back Pain (n=120), the figure shows the mean difference of all
subscales was in the limitation agreement range.
Table
3.
Item-Total correlation of Persian version of CSQ in subjects with NSCLBP
(n=120).
|
Items
|
Diverting
attention
|
Reinterpretation
|
Catastrophizing
|
Ignoring
pain
|
Praying- hope
|
self-statement
|
Increasing
Activity levels
|
|
I
3
|
0.501**
|
0.420**
|
-0.269**
|
0.385**
|
0.312**
|
0.497**
|
0.375**
|
|
I
9
|
0.443**
|
0.291**
|
0.000
|
0.237**
|
0.177
|
0.174
|
0.298**
|
|
I
12
|
0.468**
|
0.406**
|
0.074
|
0.249**
|
0.336**
|
0.315**
|
0.314**
|
|
I
26
|
0.663**
|
0.429**
|
0.027
|
0.264**
|
0.427**
|
0.404**
|
0.472**
|
|
I
27
|
0.296**
|
0.441**
|
0.148
|
0.249**
|
0.521**
|
0.493**
|
0.473**
|
|
I
38
|
0.658**
|
0.434**
|
-0.001
|
0.276**
|
0.294**
|
0.395**
|
0.343**
|
|
I
1
|
0.442**
|
0.441**
|
0.086
|
0.268**
|
0.313**
|
0.366**
|
0.193*
|
|
I
4
|
0.350**
|
0.472**
|
-0.080
|
0.330**
|
0.072
|
0.165
|
0.159
|
|
I
10
|
0.280**
|
0.445**
|
0.060
|
0.204*
|
0.190*
|
0.191*
|
0.140
|
|
I
16
|
0.432**
|
0.628**
|
0.091
|
0.346**
|
0.164
|
0.184*
|
0.336**
|
|
I
29
|
0.444**
|
0.674**
|
0.022
|
0.446**
|
0.237**
|
0.257**
|
0.352**
|
|
I
41
|
0.359**
|
0.526**
|
0.079
|
0.488**
|
0.310**
|
0.377**
|
0.438**
|
|
I
5
|
0.018
|
0.068
|
0.558**
|
-0.167
|
-0.038
|
-0.227*
|
0.046
|
|
I
11
|
-0.019
|
-0.019
|
0.667**
|
-0.209*
|
0.049
|
-0.294**
|
-0.032
|
|
I
13
|
-0.024
|
0.096
|
0.473**
|
-0.275**
|
-0.079
|
-0.330**
|
-0.034
|
|
I
25
|
0.068
|
0.120
|
0.617**
|
-0.097
|
0.393**
|
0.006
|
0.194*
|
|
I
33
|
0.012
|
0.089
|
0.667**
|
-0.128
|
0.252**
|
-0.033
|
0.218*
|
|
I
37
|
-0.016
|
0.021
|
0.588**
|
-0.227*
|
0.248**
|
-0.224*
|
0.027
|
|
I
17
|
0.291**
|
0.307**
|
-0.357**
|
0.503**
|
0.075
|
0.413**
|
0.307**
|
|
I
19
|
0.428**
|
0.496**
|
-0.092
|
0.588**
|
0.244**
|
0.446**
|
0.328**
|
|
I
21
|
0.189*
|
0.275**
|
-.243**
|
0.623**
|
0.094
|
0.392**
|
0.361**
|
|
I
24
|
0.315**
|
0.425**
|
-0.142
|
0.596**
|
0.199*
|
0.376**
|
0.357**
|
|
I
30
|
0.235**
|
0.241**
|
-0.216*
|
0.516**
|
0.180*
|
0.538**
|
0.437**
|
|
I
35
|
0.182*
|
0.353**
|
-0.171
|
0.636**
|
0.067
|
0.392**
|
0.472**
|
|
I
14
|
0.364**
|
0.224*
|
0.166
|
0.081
|
0.482**
|
0.341**
|
0.287**
|
|
I
15
|
0.296**
|
0.229*
|
0.283**
|
0.080
|
0.707**
|
0.273**
|
0.256**
|
|
I
18
|
0.550**
|
0.278**
|
0.088
|
0.226*
|
0.560**
|
0.494**
|
0.487**
|
|
I
22
|
0.329**
|
0.142
|
0.053
|
0.199*
|
0.405**
|
0.405**
|
0.316**
|
|
I
28
|
0.338**
|
0.296**
|
0.291**
|
0.127
|
0.663**
|
0.236**
|
0.263**
|
|
I
36
|
0.356**
|
0.286**
|
0.135
|
0.225*
|
0.646**
|
0.302**
|
0.333**
|
|
I
6
|
0.436**
|
0.374**
|
0.070
|
0.277**
|
0.406**
|
0.506**
|
0.365**
|
|
I
8
|
0.335**
|
0.243**
|
-0.183*
|
0.291**
|
0.437**
|
0.502**
|
0.235**
|
|
I
20
|
0.429**
|
0.246**
|
-0.233*
|
0.502**
|
0.267**
|
0.555**
|
0.341**
|
|
I
23
|
0.319**
|
0.192*
|
-0.343**
|
0.425**
|
0.230*
|
0.488**
|
0.233*
|
|
I
31
|
0.518**
|
0.403**
|
-0.160
|
0.610**
|
0.366**
|
0.666**
|
0.628**
|
|
I
32
|
0.127
|
0.012
|
-0.158
|
0.436**
|
0.170
|
0.444**
|
0.362**
|
|
I
2
|
0.303**
|
0.254**
|
0.074
|
0.296**
|
0.261**
|
0.229*
|
0.440**
|
|
I
7
|
0.267**
|
0.061
|
0.047
|
0.157
|
0.144
|
0.220*
|
0.245**
|
|
I
34
|
0.383**
|
0.278**
|
0.133
|
0.370**
|
0.291**
|
0.311**
|
0.481**
|
|
I
39
|
0.378**
|
0.351**
|
-0.043
|
0.494**
|
0.197*
|
0.403**
|
0.351**
|
|
I
40
|
0.525**
|
0.344**
|
0.101
|
0.333**
|
0.421**
|
0.418**
|
0.485**
|
|
I
42
|
0.334**
|
0.287**
|
0.085
|
0.430**
|
0.211*
|
0.362**
|
0.500**
|
In 120 patients with non-specific chronic low back pain,
the CSQ questionnaire's EFA were: The KMO test (0.753) and the Bartlett test of
sphericity (P-value = 0.000, degree of freedom = 861, Chi-square test =
56/2675) showed that the questionnaire items were appropriate for the major
component's statistical analysis. From the factor analysis, 13 factors with
eigenvalues of 10.23, 4.73, 2.44, 2.35, 1.91, 1.48, 1.36, 1.33, 1.24, 1.18,
1.15, 1.01, and 1.00 were extracted, accounting for 74.94% of the total variance.
The first factor (items 5, 11, 13, 33, 25, 37) is 24.35% of the total variance,
the second factor (items 17, 30, 31, 32, 34, 42) is 11.26% of the total
variance, the third factor (Items 18, 38, 27, 26) is 5.80% of the total
variance, the fourth factor (items 15, 28, 36) is 5.60% of the total variance,
the fifth factor (items 16, 29 and 41) is 4.5 total, the sixth factor of
variance (items 19, 21 and 24) is 3.5 total variance. The next seven factors
were composed of three (6, 7, and 8), two (22 and 14), three (23, 39, and 40),
two (9 and 12), one (10), one (4), and one (2) item, respectively. Four items
1, 3, 20, and 35 were removed due to cross-loading of Eigenvalues less than
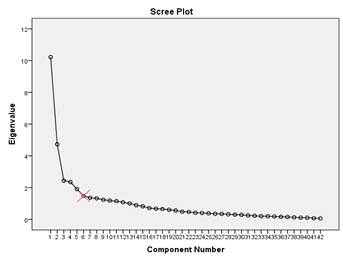
0.2. The scree plot diagram in Figure 2 shows five or six factors.
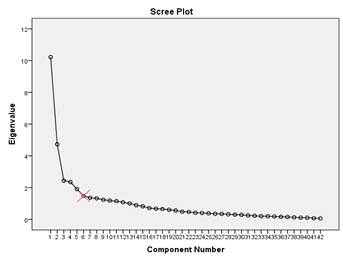
Figure 2. Scree Plot of the Persian version of CSQ
in subjects with nonspecific chronic low back pain (n=120). The red
multiplication symbol indicates the cut-off point for determining the
appropriate number of factors.
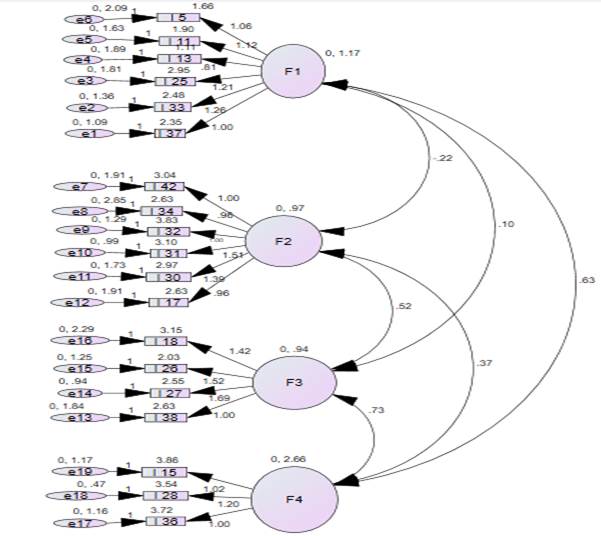
Due to the high number of factors, data simulation
was used in parallel analysis to determine the proper number of components,
which ultimately stayed at the first four. Confirmatory factor analysis yielded
the following fit indices: χ²/df = 1.77, CFI = 0.884,
TLI = 0.84, and RMSEA = 0.081. The structural equation model is depicted in
Figure 3. Table 4 shows the factor loads from the varimax-rotated matrix.
Table
4.
Factor loadings of Persian version of the CSQ in subjects with nonspecific
chronic low back pain (n=120).
|
Items
|
Factor I
catastrop-hizing
|
Factor II
Ignoring pain
|
Factor III
Diverting attention
|
Factor IV
praying
|
|
I 5
|
0.782
|
|
|
|
|
I 11
|
0.756
|
|
|
|
|
I 13
|
0.553
|
|
|
|
|
I 25
|
0.675
|
|
|
|
|
I 33
|
0.803
|
|
|
|
|
I 37
|
0.664
|
|
|
|
|
I 17
|
|
0.472
|
|
|
|
I 30
|
|
0.674
|
|
|
|
I 31
|
|
0.581
|
|
|
|
I 32
|
|
0.827
|
|
|
|
I 34
|
|
0.578
|
|
|
|
I 35
|
|
0.591
|
|
|
|
I 42
|
|
0.609
|
|
|
|
I1
|
|
|
0.435
|
|
|
I3
|
|
|
0.419
|
|
|
I 18
|
|
|
0.510
|
|
|
I 20
|
|
|
0.436
|
|
|
I 26
|
|
|
0.722
|
|
|
I 27
|
|
|
0.804
|
|
|
I 38
|
|
|
0.634
|
|
|
I 15
|
|
|
|
0.818
|
|
I 28
|
|
|
|
0.871
|
|
I 36
|
|
|
|
0.867
|
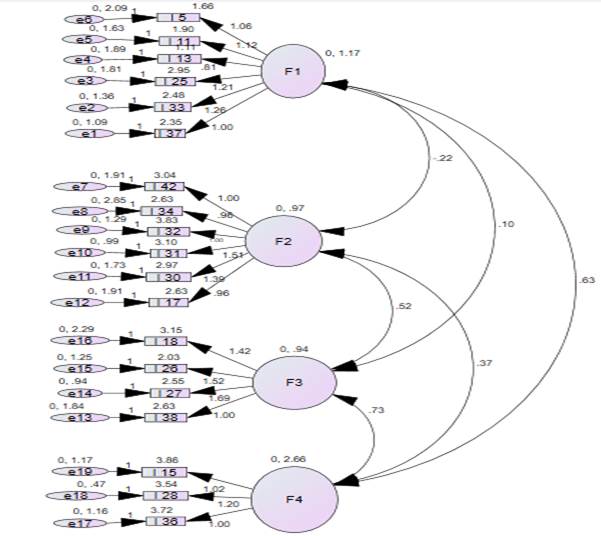
Figure
3.
the structural equation model of the Persian version of CSQ in subjects with
nonspecific chronic low back pain (n=120), The figure represents four factors
and their respective items extracted from the structural equation model of the
Persian version of CSQ.
Discussion
The four-factor structure and sufficient reliability of
the Persian version of the CSQ enable its usage in Persian-speaking
communities. Reliability and agreement: The ICC values
in this study ranged from 0.74 to 0.88 for all subscales, indicating good
reliability of the respective subscales; that is, the individual ranking in the
overall test group for two measurements has remained at an acceptable level.
The subscales' Cronbach's alpha coefficients fell between 0.7 to 0.83, which is
in line with research by Asghari, Verra, and Stoffel that found comparable
reliability ranges for the CSQ subscales (9, 10, 13). Furthermore, in this study, the CSQ subscales maintained reliable scores
when administered to 60 participants over a short test-retest interval,
mirroring results seen in both the original version and other language
adaptations of the questionnaire (5) . Although prior studies included participants with a variety of chronic
pain conditions and spinal cord injuries rather than NSCLBP specifically, their
reliability findings align closely with those of the present study,
underscoring the stability of the CSQ across populations (9, 10, 13). Additionally, the Bland-Altman plot appeared to be no obvious
bias because the mean difference was about zero. The two strategies showed good
agreement, as evidenced by the comparatively narrow limitation of agreement.
The hypothesis of good agreement was further supported by the scatter plot's
random structure (40).
The MDCs for the CSQ subscales were as follows: attention
= 9.63%, reinterpretation of pain = 7.28%, catastrophizing = 7.66%, ignoring
pain = 9.47%, praying-hope = 8.88%, self-statement = 9.08%, and increasing
activity levels = 7.43%. The MDC values indicate the minimum change needed in
subscale scores to be considered clinically meaningful. With these figures,
therapists and researchers can now interpret subscale scores in terms of their
underlying clinical importance and further establish evidence for the validity
of any change that has occurred (41).
To figure out the degree of relationship between each
item, item total correlation was also assessed. Item discrimination and each
item's connection with the overall scale were assessed using corrected
item–total score correlation (42). The Spearman correlation between each item and its matching subscale
varied from 0.358 to 0.707, according to the results shown in Table 3.
According to this finding, each item's association with its subscale was
consistently higher than its connection with other subscales. Furthermore, all
items exhibited a statistically significant correlation with their respective
subscales, with a P-value of less than 0.001.
The Persian version of the CSQ has a strong structure, as
seen by the high correlation found between its items and the associated
subscales. This close alignment between
items and subscales reinforces the validity of the Persian CSQ as a reliable
measurement tool (41).
Factor analysis: Thirteen factors were identified via
Exploratory Factor Analysis, with eigenvalues greater than 1, which explained
74.94% of the total variance. Due to the high number of factors, a parallel
analysis was performed which revealed the results for four factors. The first
factor consisted of the catastrophizing subscale items of the original version;
hence, the name “catastrophizing” was chosen. The second factor included six
items initially belonging to the ignoring pain, self-statement, and activity
increase subscales, but as all items primarily addressed ignoring pain, this
factor was named “ignoring”. The third factor consisted from three items of the
original version of the diverting attention subscale and a praying/hope
subscale item, all of which referred to diverting the individual’s attention,
so this subscale was called “the diverting attention”. The fourth factor The
fourth factor included three items from the praying/hope subscale, focusing
specifically on prayer, and was named “praying”. The four-factor model’s
goodness-of-fit results were similar to those found by Harland et al (2003) in a similar study of people with chronic low back pain. This may mean
that the type of disease affects the coping strategies that people use (15).
In a study by Tutle et al. (1991), 4 factors
(Catastrophizing, Praying and Hoping, Reinterpreting Pain Sensations, and
Diverting attention) were identified in people with chronic pain, 43% of whom
had low back pain and accidental pain (17). The results of EFA in another study on people with chronic neck pain
caused by accidents showed five factors: distraction, ignoring pain sensations,
reinterpreting pain sensations, catastrophizing, and praying and hoping (43).
In an EFA of people with fibromyalgia, Stoffel et al.
(2013) identified six factors (Catastrophizing, Ignoring Pain, Diversion,
Reinterpreting Pain Sensations, Praying, and Hoping) (13), and Harland et al. (2014) in a study that used the 24-item version in
people with low back pain also identified four factors: catastrophizing,
ignoring pain sensations, diverting attention, and reinterpreting pain
sensations (14). According to the studies mentioned above, the four factors confirmed in
this study were almost similar to those of previous studies. However, as
mentioned above, the variety of items in each factor in these studies is
different, which can be explained by the different populations, culture, and
type of disease of the participants. The consequence of culture influencing coping strategies is that a given
coping approach may be both predominant and adaptive in one culture, while just
the opposite may be the case for another. Differences in cultural approaches to
pain, rooted in historical and socio-economic contexts, probably underlie these
differences in the factor structures found in the present studies (44).
The results of confirmatory factor analysis have shown
that the 42-item version did not have an excellent fit, and the shortened
versions of 24 and 27 items had a better fit (13).
Identifying coping strategies for chronic nonspecific
back pain is important in both treatment and research. For example, van der
Hulst et al (2010) showed adaptive and maladaptive coping strategies were
associated with decreasing and increasing back muscle activity ,respectively (45) in other hand, Physical therapists can better understand the coping
strategies used by people with NSCLBP and adjust their interventions by using
the CSQ scale in rehabilitation. For patients with NSCLBP, this may result in
better functional outcomes and more efficient pain management (46). Results obtained on the CSQ scale may yield useful information about the
pain experience of the individual and aid in planning specific treatment
packages. For example, a patient who scores high on catastrophizing might
undergo rehabilitation programs with more emphasis on physical therapy and
interventions of a cognitive-behavioral nature that deal with the negative
thoughts and feelings associated with pain (47).
This study has different demographics compared to another
research. While most participants in previous studies were middle-aged males,
our sample had a higher percentage of females of lower average age. Both
studies did reveal similar internal consistency and reliability. However, there
was variation in the number of factors extracted; thus, it might be indicative
that age and gender could modify the choice of coping strategies among back
pain patients (4, 47). Further investigation on the possible relationship is required.
Limitation: Lack of confirmatory factor analysis in
another similar population and minimum sample size, lack of predictive
validity, and conducting a longitudinal study to examine changes in coping
strategies over time are among the limitations of the present study.
Conclusion
The outcomes of the current study demonstrate that the
Persian version of the CSQ is an acceptable tool for assessing coping
strategies of Iranians with chronic low back pain and it can be used in
rehabilitation clinics to identify cognitive and behavioral strategies of
patients. This questionnaire has good reliability and internal consistency. To
enhance the model’s validity, future research should conduct a secondary
confirmatory factor analysis on a new dataset. Additionally, investigating the
construct validity and responsiveness of the questionnaire would be valuable.
This comprehensive analysis would further strengthen the findings. The study’s
findings should be regarded cautiously because selection bias may have had an
impact (48).
Author
contribution
SK-GA performed
Conceptualization, Methodology, Writing - Original Draft and Investigation. BA
and MS performed Supervision and Writing - Review & Editing. ST
performed Software. AS performed Formal analysis. MS and MS
performed data collection.
Acknowledgments
The authors thank all the participants in this study.
Conflict
of interest
There
is no Conflicts of interest/competing interests.
Funding
There
is no funding.
References
1. Cabak A, et al.
Strategies for Coping with Chronic Lower Back Pain in Patients with Long
Physiotherapy Wait Time. Medical science monitor : international medical
journal of experimental and clinical research. 2015;21:3913-20.
2. Ferreira-Valente MA, et al. Psychometric
properties of the portuguese version of the Pain Self-Efficacy Questionnaire.
Acta reumatologica portuguesa. 2011;36(3):260-7.
3. Tan G, et al. Coping with chronic pain: a
comparison of two measures. Pain. 2001;90(1-2):127-33.
4. Igwesi-Chidobe CN, et al. Only two
subscales of the Coping Strategies Questionnaire are culturally relevant for
people with chronic low back pain in Nigerian Igbo populations: a
cross-cultural adaptation and validation study. Journal of patient-reported outcomes.
2021;5:1-16.
5. Rosenstiel AK, Keefe FJ. The use of coping
strategies in chronic low back pain patients: Relationship to patient
characteristics and current adjustment. Pain. 1983;17(1):33-44.
6. DeGood DE, Tait RC. Assessment of pain
beliefs and pain coping. Handbook of pain assessment. 2001;2:320-45.
7. Rodriguez Franco L, et al. [Assessment of
chronic pain coping strategies]. Actas espanolas de psiquiatria.
2004;32(2):82-91.
8. Jensen IB, Linton SJ. Coping Strategies
Questionnaire (CSQ): Reliability of the Swedish version of the CSQ. Cognitive
Behaviour Therapy. 1993;22(3-4):139-45.
9. Asghari A, Golak N. The roles of pain
coping strategies in adjustment to chronic pain. Scientific Information
Database (SID). 2005.
10. Verra ML, et al. Translation, cross-cultural
adaptation, reliability, and validity of the German version of the Coping
Strategies Questionnaire (CSQ-D). The journal of pain : official journal of the
American Pain Society. 2006;7(5):327-36.
11. Irachabal S, et al. Pain coping strategies:
French adaptation of the coping strategies questionnaire (CSQ-F). L'Encephale.
2008;34(1):47-53.
12. Spinhoven P, et al. Pain coping strategies in
a Dutch population of chronic low back pain patients. Pain. 1989;37(1):77-83.
13. Stoffel M, et al. Dimensions of coping in
chronic pain patients: factor analysis and cross-validation of the German
version of the Coping Strategies Questionnaire (CSQ-D). Rehabilitation
psychology. 2013;58(4):386-95.
14. Harland N, Martin D. Exploring the
longitudinal stability of the CSQ24 in a back pain population. Rehabilitation
psychology. 2014;59(1):79-84.
15. Harland NJ, Georgieff K. Development of the
Coping Strategies Questionnaire 24, a Clinically Utilitarian Version of the
Coping Strategies Questionnaire. Rehabilitation psychology. 2003;48(4):296.
16. Utne I, et al. Confirmatory factor analysis
of the coping strategies questionnaire-revised in samples of oncology
outpatients and inpatients with pain. Clin J Pain. 2009;25(5):391-400.
17. Tuttle DH, et al. Empirical dimensions of
coping in chronic pain patients: A factorial analysis. Rehabilitation
psychology. 1991;36(3):179.
18. Zaina F, et al. A Systematic Review of
Clinical Practice Guidelines for Persons With Non-specific Low Back Pain With
and Without Radiculopathy: Identification of Best Evidence for Rehabilitation
to Develop the WHO's Package of Interventions for Rehabilitation. Arch Phys Med
Rehabil. 2023;104(11):1913-27.
19. Misterska E, et al. Psychometric properties
of the Polish language version of the chronic pain coping inventory-42 for
patients treated surgically due to herniated lumbar discs and spondylotic
changes. Medical science monitor : international medical journal of
experimental and clinical research. 2014;20:789-801.
20. Waddell G. The back pain revolution: Elsevier
Health Sciences; 2004.
21. Chou R, et al. Diagnosis and treatment of low
back pain: a joint clinical practice guideline from the American College of
Physicians and the American Pain Society. Annals of internal medicine.
2007;147(7):478-91.
22. Koes B, et al. Diagnosis and treatment of low
back pain. BMJ. 2006;332(7555):1430.
23. Guilford J. Psychometric methods New York
McGraw-Hill, 1954. Google Scholar. 1954.
24. Kline RB. Principles and practice of
structural equation modeling: Guilford publications; 2015.
25. Hogarty KY, et al. The quality of factor
solutions in exploratory factor analysis: The influence of sample size,
communality, and overdetermination. Educational and Psychological Measurement.
2005;65(2):202-26.
26. Williams B, et al. Exploratory factor
analysis: A five-step guide for novices. Australasian Journal of Paramedicine.
2010;8(3).
27. Hair JF, et al. Multivariate data analysis:
Prentice hall Upper Saddle River, NJ; 1998.
28. Polit DF, Yang F. Measurement and the
measurement of change: a primer for the health professions: Wolters Kluwer
Health; 2015.
29. Miller MD, Ferris DG. Measurement of
subjective phenomena in primary care research: the Visual Analogue Scale.
Family practice research journal. 1993;13(1):15-24.
30. Price DD, et al. The validation of visual
analogue scales as ratio scale measures for chronic and experimental pain.
Pain. 1983;17(1):45-56.
31. Terwee CB, et al. Quality criteria were
proposed for measurement properties of health status questionnaires. Journal of
clinical epidemiology. 2007;60(1):34-42.
32. Atkinson G, Nevill AM. Statistical methods
for assessing measurement error (reliability) in variables relevant to sports
medicine. Sports medicine. 1998;26(4):217-38.
33. Weir JP. Quantifying test-retest reliability
using the intraclass correlation coefficient and the SEM. The Journal of
Strength & Conditioning Research. 2005;19(1):231-40.
34. Abad SKG, et al. Translation, reliability,
and validity of the avoidance endurance questionnaire in Iranian subjects with
chronic non-specific neck pain. Journal of Family Medicine and Primary Care.
2020;9(7):3565.
35. Howard KI, Forehand GA. A method for
correcting item-total correlations for the effect of relevant item inclusion.
Educational and Psychological Measurement. 1962;22(4):731-5.
36. Groskurth K, et al. Why we need to abandon
fixed cutoffs for goodness-of-fit indices: An extensive simulation and possible
solutions. Behav Res Methods. 2024;56(4):3891-914.
37. Monticone M, et al. The 27-item coping
strategies questionnaire-revised: confirmatory factor analysis, reliability and
validity in Italian-speaking subjects with chronic pain. Pain research &
management. 2014;19(3):153-8.
38. Roberson RB, et al. Exploratory factor
analysis in Rehabilitation Psychology: a content analysis. Rehabilitation
psychology. 2014;59(4):429-38.
39. Çokluk Ö, Koçak D. Using Horn's Parallel
Analysis Method in Exploratory Factor Analysis for Determining the Number of
Factors. Educational Sciences: Theory and Practice. 2016;16(2):537-51.
40. Seydi M, et al. Confirmatory factor Analysis,
reliability, and validity of the Persian version of the coping strategies
questionnaire for Iranian people with nonspecific chronic neck pain. Journal of
Manipulative and Physiological Therapeutics. 2021;44(1):72-84.
41. Shanbehzadeh S, et al. Reliability and
Validity of the Pain Anxiety Symptom Scale in Persian Speaking Chronic Low Back
Pain Patients. Spine. 2017.
42. Smart MH, et al. Development of an Instrument
to Assess the Perceived Effectiveness of Academic Detailing. J Contin Educ
Health Prof. 2020;40(4):235-41.
43. Swartzman LC, et al. The factor structure of
the Coping Strategies Questionnaire. Pain. 1994;57(3):311-6.
44. Orhan C, et al. Are pain beliefs, cognitions,
and behaviors influenced by race, ethnicity, and culture in patients with
chronic musculoskeletal pain: a systematic review. Pain physician.
2018;21(6):541-58.
45. van der Hulst M, et al. Back muscle
activation patterns in chronic low back pain during walking: a “guarding”
hypothesis. The Clinical journal of pain. 2010;26(1):30-7.
46. Marshall A, et al. Changes in Pain
Self-Efficacy, Coping Skills, and Fear-Avoidance Beliefs in a Randomized
Controlled Trial of Yoga, Physical Therapy, and Education for Chronic Low Back
Pain. Pain Med. 2022;23(4):834-43.
47. Sozlu U, et al. The Coping Strategies
Questionnaire: Translation, cultural adaptation, reliability and validity in
Turkish-speaking patients with chronic musculoskeletal pain. Physiotherapy
theory and practice. 2022;38(13):3090-9.
48. Dohoo IR. Bias--is it a problem, and what
should we do? Prev Vet Med. 2014;113(3):331-7.
![]() ) (32, 33).
) (32, 33).