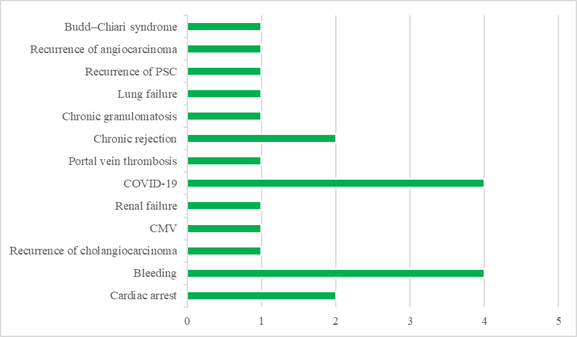
Figure 1. Comparison of
the causes of mortality (%).
The survival rate
survey of the patients undergoing liver transplants
Reyhane Ghanbari 1,2, Kourosh Mojtahedi 3,
Pirouz Samidoust 2*
1 Sajjadye Hospital, Torbat Jam
Faculty of Medical Sciences, Torbat Jam, Iran
2 Razi Clinical Research Development
Unit, Razi Hospital, Guilan University of Medical Sciences, Rasht, Iran
3 Gastrointestinal and Liver Diseases
Research Center, Guilan University of Medical Sciences, Rasht, Iran
Corresponding Authors: Pirouz
Samidoust
* Email: pirooz.samidoost@yahoo.com
Abstract
Introduction: Liver transplantation is a widely distinguished and highly practical
therapy for liver cirrhosis. In any case, liver transplant surgery assumes a
risk of influential complications. In this way, the survival rate of liver
transplant patients at Razi Healing Center in Rasht from 2017 to 2022 was
investigated.
Materials
and Methods: In this retrospective cohort study, liver transplant patients referred
to Razi Hospital in Rasht, Iran, from 2017 to 2022 were studied. Patient
demographic and clinical information were collected. Survival was determined
using Kaplan-Meier estimates. Log rank was used to determine differences
between study groups in survival.
Results: Out of 46 patients who underwent liver transplantation surgery, 54.3%
of patients survived. Also, the most common causes of death for the samples of
this study were COVID-19 and hemorrhage. Patients with autoimmune cirrhosis due
to hepatitis have a significantly higher risk of death than those with
cirrhosis due to other factors. Postoperative vascular thrombosis was found to
be significantly associated with reduced patient survival. Patient outcomes
improved significantly in the second part of the six-year liver transplant
study. The study highlights the importance of increasing experience in liver
transplant surgery and postoperative care to improve outcomes.
Conclusion: According to the results of this study, patients with autoimmune
cirrhosis due to hepatitis have a higher risk of death than those with
cirrhosis due to other causes. In addition, postoperative vascular thrombosis
is believed to significantly reduce patient survival. The study highlights the
importance of increasing experience in liver transplant surgery and
postoperative care to improve outcomes for these patients.
Keywords: Liver transplant, Surgery, Survival, Liver failure
Introduction
Liver
cirrhosis is a cancerous growth of liver cells that manifests itself as a mass
in the upper right part of the abdomen with general symptoms such as pain,
weight loss for unknown reasons, and weakness. This type of cancer occurs when
liver cells grow at an abnormal rate and form a tumor, which can be malignant
(cancerous) or benign (non-cancerous). When these cancer cells start in the
liver, they are known as primary liver cirrhosis. Hepatocellular carcinoma is a
liver cirrhosis with undifferentiated liver cells. Liver transplantation is an
elective treatment for cirrhosis, acute liver failure, and liver cirrhosis (1).
It has been demonstrated to be highly effective not only in treating acute or
chronic liver failure but also in treating primary liver cirrhosis (2). Liver
transplantation (LT) may be healing or life drawing out for suitably chosen
patients with intense liver disappointment, progressed cirrhosis, hepatic
danger, or natural metabolic disarranges. Given tremendous enhancements in
surgical methods, organ conservation and acquirement, and immunosuppression
over the past few decades, advanced LT is characterized by surprising
advancements in post-transplant persistent survival, joint survival, and
quality of life (3). The 15% mortality rate of liver transplant beneficiaries
at one year may be seen as an accomplishment in comparison with the holding up
list mortality, however, it in any case clears out room for much enhancement.
This treatment has been utilized in Iran since 1993 (4). Liver transplant recipients
are subjected to various short and long-term risks. Short-term risks are
related to technical issues, such as vascular and venous thrombosis, biliary
complications, or medical issues after transplantation, such as infection, and transplant
rejection (5). Given the severe shortage of donated organs, it is crucial to
identify patients who can benefit the most from liver transplantation in terms
of survival (6). Over 60 years have passed since the first liver transplant was
performed. The survival rate of liver transplant recipients in the first year
is 80-90%, and associated problems such as operation-induced complications,
transplant rejection, and sepsis have decreased over time (7, 8). In a study
conducted on European countries from 2002 to 2004, the 1-year and 5-year
survival rates of liver transplant recipients were reported to be 90% and 80%,
respectively (9). In another investigation in Italy, the 10-year survival rate
was found to be 72% (10). In Sabet et al.'s study, conducted in 2009, the 1-year
survival rate was 84%, while the 3-year and 6-year rates were both 82% (11).
Recognizing the predictive factors of mortality in patients with advanced liver
failure is one of the main challenges faced by researchers (10). Liver diseases
are among the most prevalent digestive diseases and account for the majority of
referrals to medical centers. A liver transplant is the primary treatment for
patients afflicted with acute or chronic liver failure. The transplantation
needs to be performed in a fully-equipped hospital and is quite costly in terms
of all types of resources. The present study aims to investigate the survival
rate of liver transplant recipients referring to Razi Hospital in Rasht, Iran
from 2017 to 2022 and also the factors associated with the survival of these
patients and better control for undesirable and intervening factors.
Materials and Methods
Statistical analysis
The normality of the data was tested using Kolmogorov-Smirnov test,
and the equality of the variances was tested using Levene’s test. Survival
rates were determined via the use of Kaplan-Meier estimates. Log-rank was
employed to determine the differences between the groups under investigation in
terms of their survival rate. The significance level was set at 0.05 for all of
the tests.
Results
During
these 5 years from 2017 to 2022, 46 patients underwent liver transplants at
Razi Hospital in Rasht, Iran. The mean age of the patients was 48.85±12.02
years. Of the total patients, 27 cases (58.7%) were male. The blood group in
47.8% of the cases was O+. Fifty-four-point-three percent of the patients were
alive until the end of the study (Table 1).
Table 1. The patient’s demographic
information and clinical/Para clinical findings.
|
Frequency and percentage |
Variable |
||
|
percentage |
Frequency |
||
|
6.5 |
3 |
< 30 |
Age group (year) |
|
41.3 |
19 |
30 – 50 |
|
|
52.2 |
24 |
> 50 |
|
|
58.7 |
27 |
Male |
Gender |
|
41.3 |
19 |
Female |
|
|
30.4 |
14 |
A+ |
Blood group |
|
19.6 |
9 |
B+ |
|
|
47.8 |
22 |
O+ |
|
|
2.2 |
1 |
A- |
|
|
54.3 |
25 |
Alive |
Outcome |
|
45.7 |
21 |
Death |
|
|
87 |
40 |
< 20 |
Meld Score |
|
13 |
6 |
> 20 |
|
|
78.3 |
36 |
No |
Background
cancer |
|
13 |
6 |
HCC |
|
|
6.8 |
3 |
Cholangiocarcinoma |
|
|
2.2 |
1 |
Angiosarcoma |
|
|
13 |
6 |
Yes |
Postoperative
thrombosis |
|
93.5 |
43 |
No |
|
|
26.1 |
12 |
Yes |
Postoperative
infection |
|
73.9 |
34 |
No |
|
|
18.2 |
8 |
Cryptogenic |
The cause of
cirrhosis |
|
30.4 |
14 |
PSC |
|
|
15.9 |
7 |
AIH |
|
|
21.7 |
10 |
NASH |
|
|
4.5 |
2 |
Biliary |
|
|
2.3 |
1 |
Wilson |
|
COVID-19
and bleeding were the most frequent causes of mortality (each of them causing 4
deaths) (Figure 1). Moreover, in one of the patients, the co-occurrence of
cholangiocarcinoma and hepatocellular carcinoma (HCC) was observed.
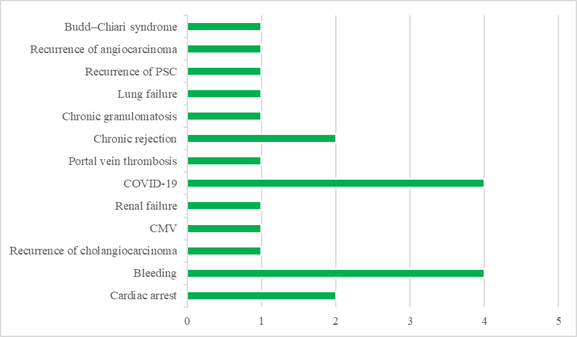
Figure 1. Comparison of
the causes of mortality (%).
Patients with
autoimmune hepatitis-induced cirrhosis were at significantly greater risk of
death compared to those whose cirrhosis was induced by other factors (Table 2).
Table 2. Comparison of the variables based on the outcome of the disease.
|
P |
Frequency and percentage |
Variable |
||
|
Death |
Alive |
|||
|
0.148 |
3 (100) |
0 |
< 30 |
Age group (year) |
|
8 (42.1) |
11 (57.9) |
30 – 50 |
||
|
10 (41.7) |
14 (58.3) |
> 50 |
||
|
0.162 |
10 (37) |
17 (63) |
Male |
Gender |
|
11 (57.9) |
8 (42.1) |
Female |
||
|
0.392 |
5 (35.7) |
9 (64.3) |
A+ |
Blood group |
|
6 (77.7) |
3 (33.3) |
B+ |
||
|
10 (45.5) |
12 (54.5) |
O+ |
||
|
0 |
1 (100) |
A- |
||
|
0.268 |
17 (42.5) |
23 (57.5) |
< 20 |
Meld Score |
|
4 (66.7) |
2 (33.3) |
> 20 |
||
|
0.549 |
16 (44.4) |
20 (55.6) |
No |
Background
cancer |
|
3 (42.9) |
4 (57.1) |
HCC |
||
|
2 (66.7) |
1 (33.3) |
Cholangiocarcinoma |
||
|
1 (100) |
0 |
Angiosarcoma |
||
|
0.047 |
5 (83.3) |
1 (16.7) |
Yes |
Postoperative
thrombosis |
|
16 (40) |
24 (60) |
No |
||
|
0747 |
5 (41.7) |
7 (58.3) |
Yes |
Postoperative
infection |
|
16 (47.1) |
18 (52.90 |
No |
||
|
0.222 |
2 (25) |
6 (75) |
Cryptogenic |
The cause of
cirrhosis |
|
0.336 |
8 (57.1) |
6 (46.9) |
PSC |
|
|
0.021 |
6 (85.7) |
1 (14.3) |
AIH |
|
|
0.685 |
3 (40) |
6 (60) |
NASH |
|
|
0.900 |
1 (50) |
1 (50) |
Biliary |
|
|
0.354 |
0 |
1 (100) |
Wilson |
|
Based on the results obtained from the log-rank test, vascular
thrombosis after surgery was found to be significantly associated with a
decrease in the patient’s survival (Table 3).
Table 3. Results of log-rank
test based on the variables under investigation.
|
P |
std. error |
Estimate |
Variable |
|
|
0.58 |
1.63 |
3 |
< 30 |
Age group (year) |
|
1.08 |
8 |
30 – 50 |
||
|
4.28 |
7 |
> 50 |
||
|
0.04 |
3.63 |
12 |
Male |
Gender |
|
2.17 |
4 |
Female |
||
|
0.95 |
1.82 |
7 |
A+ |
Blood group |
|
2.98 |
3 |
B+ |
||
|
1.53 |
9 |
O+ |
||
|
- |
8 |
A- |
||
|
0.59 |
1.35 |
8 |
< 20 |
Meld Score |
|
0 |
1 |
> 20 |
||
|
0.44 |
1.19 |
7 |
No |
Background cancer |
|
2.61 |
20 |
HCC |
||
|
9.79 |
15 |
Cholangiocarcinoma |
||
|
- |
18 |
Angiosarcoma |
||
|
0.003 |
1.22 |
2 |
Yes |
Postoperative thrombosis |
|
2.52 |
9 |
No |
||
|
0.68 |
4.33 |
4 |
Yes |
Postoperative infection |
|
1.45 |
8 |
No |
||
|
0.45 |
2.82 |
7 |
Cryptogenic |
The cause of cirrhosis |
|
1.52 |
8 |
|||
|
0.78 |
1.87 |
6 |
Primary
sclerosing cholangitis (PSC) |
|
|
1.97 |
9 |
|||
|
0.003 |
1.19 |
3 |
Autoimmune hepatitis (AIH) |
|
|
3.12 |
9 |
|||
|
0.16 |
3.16 |
20 |
Non-alcoholic steatohepatitis (NASH) |
|
|
1.19 |
7 |
|||
|
0.30 |
- |
1 |
Biliary |
|
|
1.42 |
8 |
|||
|
0.95 |
- |
14 |
Wilson |
|
|
1.27 |
8 |
|||
The findings presented in Table 4 indicate that patient outcomes
improved significantly in the 2nd part of the 6 years of liver
transplant under investigation in this study as compared to its 1st
part. More specifically, the survival rate of the patients undergoing liver
transplantation in the 2nd triennium was more than twice as much as
that in the 1st triennium (70.4% vs. 31.6%, respectively). This
might be because the department of liver transplant in this medical center was
newly established at that time. Later, with further developments in the
department as well as the employment of a fellow in liver transplant, the patient’s
outcomes improved significantly.
Table 4. Comparison of
patients’ outcomes in the 1st and 2nd triennium of liver
transplant at Razi Hospital in Rasht.
|
P |
Outcome |
Frequency and percentage |
Year of transplantation |
|
|
Death |
Alive |
|||
|
0.009 |
13 (68.4) |
6 (31.6) |
19 (41.3) |
2017 - 2019 |
|
8 (29.6) |
19 (70.4) |
27 (58.7) |
2020 - 2023 |
|
|
|
21 (45.7) |
25 (54.3) |
46 (100) |
Sum |
Discussion
Liver transplant has been used in Iran as a therapy for over two decades.
In this study, a total of 46 liver transplant patients were investigated. The
mean age of the patients was 48.85±12.02 years. The patients’ survival was
80.43% in the first month, 36.95% in the first year, and 8.69% in the 3 years
after the surgery. Germani et al. conducted a study to analyze donor, graft,
and recipient variables from the European Liver Transplant Registry database
between January 1988 and June 2009. The study compared etiologies and periods
and generated separate training datasets to develop three- and 12-month
survival models, which were then validated. A sub-analysis was conducted for
recipients older than 50 years.The results of the study showed that out of
4,903 patients evaluated, the one-, five-, and ten-year patient and graft
survival rates were 74%, 68%, 63%, 63%, 57%, and 50%, respectively. Despite an
increase in donors over 60 years from 1.8% to 21%, survival rates were better
in the 2004-2009 period than in previous periods (p<0.001). In addition, the
study found that paracetamol-related acute liver failure had a higher incidence
of suicide or non-adherence (p<0.001).Furthermore, male recipients, recipients
aged over 50 years, incompatible ABO matching, donors over 60 years, and reduced
size were independently associated with death or graft loss. In conclusion,
despite increases in donor/recipient age, survival after liver transplantation
has improved. However, the study suggests that recipients over 50 years paired
with donors over 60 years had a very high mortality/graft loss within the first
year (11). Bertacco and colleagues conducted a study that analyzed a
prospective database of liver transplantation in adult recipients who passed
away within three months following the procedure. Of the 335 liver transplants
performed during the study period (2012 -2016), 24 adults and two pediatric
patients died within 90 days. According to the study's results, sepsis was
identified as the leading cause of early mortality following liver
transplantation. The study further highlighted that infections were the primary
cause of morbidity and mortality in LT recipients, with 80% of patients
experiencing at least one infective episode within the first year. Bacteremia,
which was primarily caused by respiratory or abdominal infections due to
drainage or vascular access, typically arose during the first 90 days after
transplantation. Mortality rates varied from 24% to 36% but rose to 50% in
cases where the septic shock was present (12). In another study by Vincenzo
Mazzaferro, liver transplantation for hepatocellular carcinoma is evolving and
the so-called expanded criteria are still being debated. This study aimed to
investigate the effectiveness of liver transplantation after the successful
removal of hepatocellular carcinoma. Patients aged 18 to 65 years with
hepatocellular carcinoma beyond Milan criteria, absence of macrovascular
invasion or extrahepatic spread, estimated 5-year post-transplant survival of
at least 50%, and good liver function (Child-Pugh A-B7) were selected. In this
study, they concluded that after effective and stable resection of eligible
hepatocellular carcinomas beyond the Milan criteria, liver transplantation
improved tumor event-free survival and overall survival compared with
non-transplant therapy after tumor response staging, which could be Expanding
criteria for hepatocellular carcinoma transplantation will help (13). In a
study conducted by Kyoung-Sun Kim et al., electrocardiography (ECG) is
routinely performed as a preoperative cardiac evaluation tool, and the effect
of myocardial ischemia detected by ECG on postoperative outcomes is uncertain.
This evaluation aimed to use ECG as a predictor of postoperative mortality in
patients undergoing patient transplantation. Electronic medical records of
patients undergoing LT were retrospectively reviewed and analyzed. The primary
endpoint was 1-year postoperative mortality. Of 1430 patients, 78 (5.5%) showed
ischemic changes in ECG. The 1-year mortality of patients with an ischemic
change on the ECG was significantly higher than that of patients without it
(11.5% vs. 4.0%; P ¼ 0.004). In a Cox proportional hazards model, ischemic
change in ECG (hazard ratio [HR], 2.91; 95% CI, 1.43–5.92; P ¼ 0.003), modeled
for end-stage liver disease score (HR 1.06; 95% CI CI: 1.09–1.04; P < .001),
and revised cardiac risk index (HR, 2.84; 95% CI, 1.86–4.35; P < .001) were
independent predictors of mortality. They were one year old. However, MPS
abnormality and echocardiographic wall motion abnormalities were absent. This
study concluded that in patients undergoing LT, preoperative ischemic ECG
findings should not be ignored, as they are associated with increased
mortality, and thorough evaluations for the diagnosis of coronary artery
disease are warranted in patients with these findings (14). Rana and colleagues
conducted the taking after considering the point of the mortality rates to
distinguish high-risk periods and to join the cause of passing into the
examination of post-transplant survival. They performed a review investigation
on joined together Organize for Organ Sharing information for all grown-up
beneficiaries of liver transplants from January 1, 2002, to October 31, 2011.
Our examination included multivariate calculated relapse where the essential
result degree was persistent passing of 49 288 beneficiaries. The most
noteworthy mortality rate by day post-transplant was on the day (0.9%). The
foremost noteworthy chance components were as follows: for one mortality from
specialized disappointment, intensive care unit confirmation chances proportion
(OR 3.2); for one mortality from unite disappointment, warm ischemia >75 min
(OR 5.6); for one-month mortality from contamination, a past transplant (OR
3.3); and for one-month mortality from join disappointment, a past transplant
(OR 3.7). They found that the most elevated mortality rate after liver
transplantation is inside the primary day and the primary month
post-transplant. Those two high-risk periods have common, as well as diverse,
chance components for mortality (15). The study conducted by Watt et al.
analyzed The National Institute of Diabetes and Digestive and Kidney Diseases
LT Database of 798 liver transplant recipients who underwent the procedure
between 1990 and 1994, with follow-up until 2003. The study found that out of
the recipients, 327 died, with the leading causes of death after one year being
hepatic, malignancy, cardiovascular disease, infection, and renal failure.
Furthermore, the incidence of renal-related death increased significantly over
time. (16). A. Bertacco et al Check out a review observational examination of
grown-up patients who experienced LT within the period 2012 to 2016 and passed
on within 90 days after LT was conducted. Prohibition criteria were
intraoperative passing, part liver, and domino transplant. Passing was
considered a subordinate variable and classified into 3 diverse bunches:
passing by sepsis, vascular occasions not related to the unit, and essential
non-function. Giver and beneficiary factors were considered and analyzed
utilizing Fisher's correct test. Significant affiliations (P esteem < .05)
were found between renal work bolster, transplantation, and the number of new
solidified plasma units transfused in one bunch and early passing due to sepsis
within the other. The hypothesis of distinguished a few chance variables
related to the particular cause of early passing in liver transplantation. The
clinical suggestions of these discoveries are the capacity to stratify patients
at a higher chance of early passing by arranging more serious and exact
administration for them (17). In the
study conducted by Salizzoni et al., 1000 liver transplant surgeries performed
on 910 patients mainly suffering from cirrhosis were investigated. The overall
1-year, 5-year, and 10-year survival rates were found to be 87%, 78%, and 72%,
respectively (9). It seems that the survival rate of liver transplant patients
is affected by several factors (11, 12, 16).
In the current study, 21.6% of the patients had underlying cancer, which
could lower their survival. Another important issue was that this study was
conducted during the COVID-19 pandemic in Iran, which could lead to an increase
in the mortality of the patients under investigation. David P. Vogt et al.,
analysis included 433 patients who survived at least 1 year after liver
transplantation from November 1, 1984, to December 31, 2001. In total, 586
liver transplants were performed. This period. The 1-, 5-, and 10-year overall survival rates as
well as the 5- and 10-year survival rates of patients who survived one year
were analyzed based on Kaplan-Meier
survival estimates. Variables inspected included determination, sex, age, and
transplantation. The causes of passing were moreover analyzed. By and large 1, 5, and 10-year survivals were
85%, 73%, and 55%, respectively. The 5 and 10-year survivals for those patients
who lived for a year were 86% and 65%, respectively. Fifty-one percent of the
causes of late passing were graft-related, 71% from repetitive essential
illness. Cardiovascular occasions and de novo malignancies were mindful for 65%
of the no graft-related passing. At last, the long-term survival in patients
who survive for the primary year after liver transplantation is fabulous.
Repetitive essential illness is mindful of the larger part of graft-related
passing. Cardiovascular occasions and de novo threat cause most of the no
graft-related passing (18).In a similar investigation between 1989 and July
2010, all patients who kicked the bucket three months after liver
transplantation were included. Statistic characteristics, preoperative and
preoperative information, benefactor characteristics, postoperative
complications, and causes of mortality were collected. Among the 788 performed
liver transplantations, 76 patients kicked the bucket in the serious care unit
(11%). The most common signs of liver transplantation were alcoholic cirrhosis
(30%), hepatitis C (28%), hepatocarcinoma (15%), and primitive or auxiliary
biliary cirrhosis (10%). Fifty percent of the patients were categorized as
Child C. The most causes of passing were non-function or brokenness with
transplantation contra-indication unite (18%), sepsis (18%), neurological
complications (12%), hemorrhagic stun (13%), (9%), multiorgan disappointments
(5%), cardiac complications (6%). These come about to emphasize the need for
superior control of sepsis, discharge, and immunosuppresses (19).
Conclusions
The results of the present study
indicated that patient outcomes improved significantly in the 2nd
part of the 6 years of liver transplant under investigation in this study as
compared to its 1st part. More specifically, the survival rate of
the patients undergoing liver transplantation in the 2nd triennium
was more than twice as much as that in the 1st triennium (70.4% vs.
31.6%, respectively). This might be because the department of liver transplant
in this medical center was newly established at that time. Later, with further
developments in the department as well as the employment of a fellow in liver
transplant, the patient’s outcome improved significantly.
Regarding the increase in the cases of
acute or chronic liver failure and because liver transplant is the final
treatment for most of these cases, it seems that in addition to the development
of liver transplant centers, increasing experience in liver transplant surgery
and postoperative care will improve outcomes.
Author contribution
RGH, KM, and PS prepared, coded, and validated all
figures and wrote the original manuscript. RGH and PS analyzed
the data. KM and PS did the research and methodology. Then, they
managed, modified, and edited the manuscript from scientific and technical
points of view. All authors read the manuscript in full and approved the final
edited version.
Acknowledgments
The authors thank Guilan University of Medical Sciences for
undertaking the study and the personnel of the Clinical Research Development
Unit of Razi Hospital in Rasht (North of Iran) for their unwavering cooperation
in performing this study.
Conflict of interest
The authors declare that they have no competing interests.
Funding/Support
This research did not receive any specific grant from funding agencies
in the public, commercial, or not-for-profit sectors.
References
1. Fox
AN, Brown RS Jr. Is the patient a candidate for liver transplantation? Clin
Liver Dis. 2012 May;16(2):435-48.
2. Da Silva RX,
Muellhaupt B, Dutkowski P, Clavien PA. Liver transplantation for malignant
liver tumors. iLIVER. 2022 Mar 1;1(1):3-11.
3. Berg CL.
Liver Transplantation in 2016: An Update. N C Med J. 2016 May-Jun;77(3):194-7.
4. Gonwa TA,
Klintmalm GB, Levy M, Jennings LS, Goldstein RM, Husberg BS. Impact of
pretransplant renal function on survival after liver transplantation.
Transplantation. 1995 Feb 15;59(3):361-5.
5. Mohan BP,
Iriana S, Khan SR, Yarra P, Ponnada S, Gallegos-Orozco JF. Outcomes of liver
transplantation in patients 70 years or older: a systematic review and
meta-analysis. Ann Hepatol. 2022 Nov-Dec;27(6):100741.
6. Delmonico
FL, Jenkins RL, Freeman R, Vacanti J, Bradley J, Dienstag JL, Trey C, Lewis WD,
Lillehei CW, Auchincloss H Jr, et al. The high-risk liver allograft recipient.
Should allocation policy consider outcome? Arch Surg. 1992 May;127(5):579-84.
7. Meirelles
Júnior RF, Salvalaggio P, Rezende MB, Evangelista AS, Guardia BD, Matielo CE,
Neves DB, Pandullo FL, Felga GE, Alves JA, Curvelo LA, Diaz LG, Rusi MB,
Viveiros Mde M, Almeida MD, Pedroso PT, Rocco RA, Meira Filho SP. Liver
transplantation: history, outcomes and perspectives. Einstein (Sao Paulo). 2015
Jan-Mar;13(1):149-52.
8. Zarrinpar A,
Busuttil RW. Liver transplantation: past, present and future. Nat Rev
Gastroenterol Hepatol. 2013 Jul;10(7):434-40.
9. Salizzoni M,
Cerutti E, Romagnoli R, Lupo F, Franchello A, Zamboni F, Gennari F, Strignano
P, Ricchiuti A, Brunati A, Schellino MM, Ottobrelli A, Marzano A, Lavezzo B,
David E, Rizzetto M. The first one thousand liver transplants in Turin: a
single-center experience in Italy. Transpl Int. 2005 Dec;18(12):1328-35.
10. Adam R,
Cailliez V, Majno P, Karam V, McMaster P, Caine RY, O'Grady J, Pichlmayr R,
Neuhaus P, Otte JB, Hoeckerstedt K, Bismuth H. Normalised intrinsic mortality
risk in liver transplantation: European Liver Transplant Registry study.
Lancet. 2000 Aug 19;356(9230):621-7.
11. Germani G,
Theocharidou E, Adam R, Karam V, Wendon J, O'Grady J, Burra P, Senzolo M, Mirza
D, Castaing D, Klempnauer J, Pollard S, Paul A, Belghiti J, Tsochatzis E,
Burroughs AK. Liver transplantation for acute liver failure in Europe: outcomes
over 20 years from the ELTR database. J Hepatol. 2012 Aug;57(2):288-96.
12. Bertacco A,
Barbieri S, Guastalla G, Boetto R, Vitale A, Zanus G, Cillo U, Feltracco P.
Risk Factors for Early Mortality in Liver Transplant Patients. Transplant Proc.
2019 Jan-Feb;51(1):179-183.
13. Mazzaferro
V, Citterio D, Bhoori S, Bongini M, Miceli R, De Carlis L, Colledan M,
Salizzoni M, Romagnoli R, Antonelli B, Vivarelli M, Tisone G, Rossi M,
Gruttadauria S, Di Sandro S, De Carlis R, Lucà MG, De Giorgio M, Mirabella S,
Belli L, Fagiuoli S, Martini S, Iavarone M, Svegliati Baroni G, Angelico M,
Ginanni Corradini S, Volpes R, Mariani L, Regalia E, Flores M, Droz Dit Busset
M, Sposito C. Liver transplantation in hepatocellular carcinoma after tumour
downstaging (XXL): a randomised, controlled, phase 2b/3 trial. Lancet Oncol.
2020 Jul;21(7):947-956.
14. Kim KS,
Park YS, Moon YJ, Jung KW, Kang J, Hwang GS. Preoperative Myocardial Ischemia
Detected With Electrocardiography Is Associated With Reduced 1-Year Survival
Rate in Patients Undergoing Liver Transplant. Transplant Proc. 2019
Oct;51(8):2755-2760.
15. Rana A,
Kaplan B, Jie T, Porubsky M, Habib S, Rilo H, Gruessner AC, Gruessner RW. A
critical analysis of early death after adult liver transplants. Clin
Transplant. 2013 Jul-Aug;27(4):E448-53.
16. Watt KD,
Pedersen RA, Kremers WK, Heimbach JK, Charlton MR. Evolution of causes and risk
factors for mortality post-liver transplant: results of the NIDDK long-term
follow-up study. Am J Transplant. 2010 Jun;10(6):1420-7.
17. Bertacco A,
Barbieri S, Guastalla G, Boetto R, Vitale A, Zanus G, Cillo U, Feltracco P.
Risk Factors for Early Mortality in Liver Transplant Patients. Transplant Proc.
2019 Jan-Feb;51(1):179-183.
18. Vogt DP,
Henderson JM, Carey WD, Barnes D. The long-term survival and causes of death in
patients who survive at least 1 year after liver transplantation. Surgery. 2002
Oct;132(4):775-80; discussion 780.
19. Jung B,
Cisse M, Chanques G, Arsac E, Bismuth M, Panaro F, Perrigault PF, Souche B,
Gallix B, Verzilli D, Delay JM, Navarro F, Pageaux GP, Jaber S. Mortalité trois
mois après transplantation hépatique : étude monocentrique sur une période
de vingt ans [Causes of early mortality after liver transplantation: a
twenty-years single centre experience]. Ann Fr Anesth Reanim. 2011
Dec;30(12):899-904.