Frequency of adult
attention deficit hyperactivity disorder (ADHD) in outpatient psychiatric
clinic, Babol University of Medical Sciences
Sakineh Javadian 1, Seyedeh Maryam
Zavarmosavi 2, Mohsen Ashrafi 3, Hemmat Gholinia 4,
Armon Massoodi 5 *
1 Department of Psychiatry, School of Medicine, Social
Determinants of Health Research Center, Health Research Institute, Babol
University of Medical Sciences
2 Department
of Psychiatry, Shafa Hospital, Guilan University of Medical Sciences, Rasht,
Iran
3 Student Research Committee, Babol University of
Medical Sciences, Babol, Iran
4 Health Research Institute, Babol University of
Medical Sciences, Babol, Iran
5 Social Determinants of Health Research Center, Health
Research Institute, Babol University of Medical Sciences, Babol, Iran
Corresponding Authors: Armon
Massoodi
* Email: armonmassoodi@gmail.com
Abstract
Introduction: Attention Deficit Hyperactivity Disorder (ADHD) in adulthood is
associated with significant impairment in occupational, academic, and social
functioning. The aim of this study is to survey the frequency of ADHD in adults
referred to psychiatric clinics.
Methods: The present
cross-sectional descriptive study includes 300 patients referred to psychiatric
clinics affiliated to Babol University of Medical Sciences with an age range of
18-45 years who were selected and included in the study. It is used the adults
Attention Deficit Hyperactivity Disorder self-report scale (ASRS V1.1) to
diagnose Adult ADHD in these individuals. Logistic regression and P-Paired test
were used to analyze the data.
Results: The mean age of the subjects was 30.21 ± 7 7.94. Of these, 181 (60.3%)
were men and 119 (39.7%) were women. The overall prevalence of Adult ADHD in
the study samples was 39.3%. In the logistic regression analysis of crude and
adjusted data of study variables, no significant relationship was seen between
Adult ADHD and age, education, employment status and marital status (P ≥ 0.05),
but a significant relationship between Adult ADHD and consumption of
Cigarettes, alcohol and drugs were observed (P ≤ 0.05).
Conclusion: The findings of the present study show a relatively high prevalence of
Adult ADHD among people with a history of psychiatric disorder, who are more
likely to be exposed to smoking, alcohol and drug abuse.
Keywords: Attention Deficit Hyperactivity Disorder, Mental Disorder, Adult
Introduction
Adult
ADHD is a type of psychiatric disorder that often appears in childhood. It is
characterized by a stable pattern of attention deficit, hyperactivity, and
impulsive behaviors (1). Impulsive behaviors are performed momentarily, without
thinking about their results and without analyzing and evaluating positive and
negative achievements. Attention-deficit/hyperactivity disorder is known as a
childhood disorder that can be improved with supervision and treatment, but
many sources have shown that ADHD is stable in adulthood and difficult to treat
(2,3). Executive functions that may be abnormal in adults with ADHD include
working memory, task switching, self-monitoring, initiation, and self-control.
These deficits are related to the attention deficit. Characterize Adult ADHD
problems: concentrating on a specific task, especially for long periods,
organizing activities, prioritizing tasks, following up and completing tasks,
forgetfulness, time management (as example of missing an appointment) (4).
Adults with Adult ADHD often report that things only get done at the last
minute, often late or not at all. An increase in driving-related problems,
including an increase in driving errors, traffic fines, and speeding, may be
related to attention deficits (5).
Adults
with ADHD have higher rates of employment problems, criminal activity,
substance abuse problems, accidents, and vehicular referrals compared to adults
without ADHD. It is believed that ADHD-related disorders from childhood such as
academic problems, self-esteem problems significantly in family and peer
relationships underlie these behavioral problems in adulthood (6). Mortality
rates were higher than in people with ADHD compared to people without ADHD in a
study in 2015 using Danish national registry data, with accidents being the
most common cause of death in people with ADHD (7).
ADHD
is a common disorder among young people worldwide. In a study in 2007, a
meta-analysis of more than 100 studies estimated the prevalence of ADHD in
children and adolescents worldwide at 5.3% (8). Simon et al., found the
prevalence of ADHD to be 2.5% in adults based on a meta-analysis of six studies
(9). Prospective longitudinal studies support the theory that approximately
two-thirds of adolescents with ADHD retain symptoms of the disorder into
adulthood (10). Recent changes in the new DSM-5 diagnostic criteria have
increased the prevalence of ADHD, which is less significant for children but
has likely had a significant impact on diagnosis rates in adults (11, 12). In a
World Health Organization survey, among respondents aged 18 to 44 in ten
countries in the Americas, Europe, and the Middle East, the current prevalence
of ADHD in adults was assessed 3.4%, which was 1.9% in low-income countries and
4.2% in high-income countries (13).
ADHD
is associated with a number of psychiatric illnesses. It has been reported that
approximately 80% of adult ADHD patients have at least one lifelong psychiatric
illness in adults. Major depressive disorder (MDD) is the most common
comorbidity (prevalence 24.4 to 31%) (14). Anxiety disorders are also a common
disease of adult ADHD patients. In the general population, the prevalence of
any anxiety disorder approaches 20%, while this figure increases to 47% in
adults with Adult ADHD (15). In addition, 65% of adult patients with adult ADHD
and concurrent bipolar disorder have a history of at least one anxiety disorder
during their lifetime (16). Substance abuse is another common comorbidity seen
in adult ADHD patients, who may use alcohol, drugs, and nicotine as a form of
self-medication (17). It has been estimated that approximately one-fourth of
people with substance use disorder (SUD) have co-occurring ADHD, and in
addition, they have a worse treatment prognosis compared to substance abusers
without adult ADHD (18). There is evidence that ADHD treatment in childhood or
adolescence may reduce the severity and course of substance use disorders in
adulthood (19).
Perhaps
the most serious aspect of ADHD lies in its tendency to be associated with
disorders, some of which affect not only behavior but also personality. This
not only endangers the well-being and life of ADHD sufferers but also their
social environment. These comorbidities are seen in children and if not
resolved in late puberty, they can turn into personality disorders such as
antisocial personality disorder or continue as extroversion disorders until
adulthood (20). Sleep disorders are another comorbidity that affects children
with ADHD at a much higher level than developing children (21). In addition,
these sleep disturbances can exacerbate ADHD symptoms such as inattention and
motor dysfunction even more (22).
Vnukova
et al., in 2020 conducted a study in the Czech population to investigate the
prevalence of ADHD among adults. It was observed that 119 (7.84%) of 1518
people were diagnosed with ADHD based on the ASRS questionnaire. Also, the rate
of ADHD was higher in men than in women. The age of subjects was also related
to ASRS score (23). In 2018, Valsecchi et al conducted a study to determine the
prevalence and clinical correlates of Adult ADHD in a sample of psychiatric
outpatients. Their study included 634 outpatients and they used the ASRS
questionnaire and DIVA specialized calculator to diagnose ADHD. The findings of
the study showed that 12.8% of people were considered ADHD-positive in the ASRS
questionnaire and 6.9% of people based on the DIVA specialized interview (24).
According to the mentioned issues, Adult ADHD has a great psychological and
social burden for the individual and society. On the other hand, due to the
relationship between Adult ADHD and various comorbidities, it is possible to
reduce the psychological and social burden of the disease in people who go to
the doctor because of other psychiatric disorders. In addition, due to its
relatively high prevalence in adults and the fact that in many children, the
symptoms continue until adulthood, and in the adult period, less importance is
given to its diagnosis and treatment, and this issue can have many consequences
for the affected person, his/her family and the community and cause problems
such as job problems, marital problems and delinquency. The present study aims
to investigate the frequency of adult attention deficit hyperactivity disorder
(Adult ADHD) in outpatients of the psychiatric clinic of Babol University of
Medical Sciences.
Methods
The
current descriptive-cross-sectional study was conducted with the aim of
investigating the frequency of adult attention deficit hyperactivity disorder
(Adult ADHD) in the outpatients of the psychiatric clinic of Babol University
of Medical Sciences. The research samples were selected using available
sampling method, including 300 patients who visited the psychiatric clinics of
Babol University of Medical Sciences as outpatients in the period of autumn
2019. Inclusion criteria include the age range of 18 to 45 years, absence of
severe mental disability and psychotic disorder, cognitive impairment,
willingness and consent to participate in the study. The only exclusion
criterion of the study includes unwillingness to continue cooperating in the
study.
Sample
volume calculation formula:
n =
sample size = 300
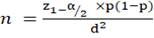 (1)
(1)
In
relationship (1)
α =
0.05
p
=0.1
d
=0.025
z =
percentage of standard error of the acceptable confidence factor
p =
proportion of the population with a given trait
q=1-p
A proportion of the population without a certain trait
α=
degree of confidence or desired possible accuracy
d=
maximum sampling accuracy
Sampling
and distribution of the questionnaire was done after obtaining permission from
the Vice-Chancellor of Research and obtaining a research permit and code of
ethics IR.MUBABOL.REC.1399.242 and obtaining permission from the responsible
director and head of the psychiatric clinic of Babol University of Medical
Sciences and explaining the research objectives to them. The questionnaires
were completed by the researcher himself, and in order to preserve the
confidentiality of the information of the research samples, the questionnaires
were without names. The reason for using this method is that if the samples had
problems in understanding the sentences of the questionnaire, sufficient
explanations would be given to them. First, the research samples were talked to
and the necessary explanations were given to these people about the research,
its necessity and benefits.
Then,
if they were satisfied and completed the written consent form, they answered
the study questionnaires. In the present study, there are two questionnaires,
in which form number 1 deals with the demographic characteristics of the
individual, and in form number 2, all patients completed the self-report
questionnaire of adult attention deficit hyperactivity disorder (ASRS-v.1.1).
Demographic
information including age, sex, occupation, education, as well as clinical
records such as physical illness records, psychiatric illness and
hospitalization records, history of referral or treatment for ADHD in
childhood, duration of drug use, type of drug used were collected from all
patients. The Adult Attention Deficit Hyperactivity Disorder Self-Report Scale
(ASRS-v.1.1) was developed by the World Health Organization (WHO) and a working
group consisting of teams of psychiatrists and researchers from the World
Health Organization. ASRS scale questions are consistent with DSM-5 criteria.
This scale includes two dimensions and 18 questions, which are divided into two
parts, A and B. There are 9 questions for the dimension of inattention and 9 questions
for the dimension of hyperactivity/impulsivity. Research questions are scored
on a 5-point Likert scale from never (1 point) to almost always (5 points). In
a study conducted in Iran by Mokhtari et al., the reliability of the
questionnaire using Cronbach's alpha method was 87%. Also, the sensitivity of
this questionnaire with a cut-off point of 50 for diagnosing ADHD in adults is
70% and the specificity of this questionnaire is 99% (25).
After
completing the questionnaires by the research samples, the score of the ASRS
questionnaire is calculated and people with a score less than 50 are considered
not suffering from Adult ADHD, and people with a score of 50 and above are
considered suffering from Adult ADHD.
The
resulting data were entered into SPSS statistical software version 24 and
evaluated quantitatively and qualitatively. The significant level of the test
will be less than 0.05 (p<0.05). P-Paired and Chi-square statistical tests
were used to analyze the data.
Results
This
cross-sectional study was conducted on 300 people who referred to psychiatric
clinics affiliated to Babol University of Medical Sciences to determine the
frequency of Adult ADHD in adults. All the study samples have answered the
answer letters completely and are in accordance with the entry and exit
criteria of the study. For this reason, we did not have a sample excluded from
the study.
The
average age of the subjects was 30.21 years with a standard deviation of 7.94.
181 cases (60.3%) were men and 119 cases (39.7%) were women. 43 cases (14.3%)
had a bachelor's degree, 103 cases (34.3%) had diploma education and 154 cases
(51.3%) had higher education. 214 cases (71.3%) were employed and the rest were
unemployed, 157 cases (52.3%) were single and 143 cases (47.7%) were married.
In addition, 51 cases (17%) had a history of using at least one of tobacco,
alcohol or drugs. In connection with the use of the mentioned items, 49 cases
(16.3%) used tobacco, 17 cases (5.7%) used alcohol, and 15 cases (5%) also used
drugs.
Logistic
regression analysis was used to investigate adult ADHD and risk factors
affecting it. People with a score of 50 and above were considered to have Adult
ADHD and people with a score below 50 were considered not to have Adult ADHD.
Also, the average adult ADHD score of people in general was 46.7 with a
standard deviation of 11.08 and 118 people (39.3%) had adult ADHD and 182
people (60.7%) did not have adult ADHD.
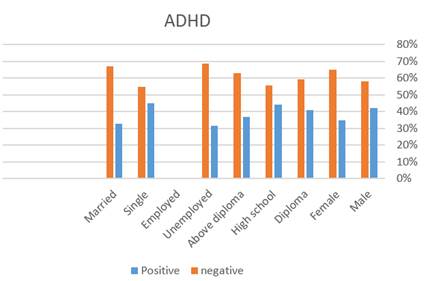
The
findings related to data analysis and their relationship with adult ADHD are
given in Table 1 and Figure 1.
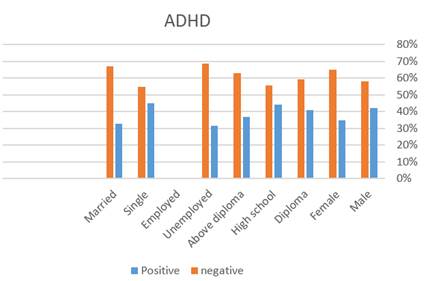
Figure
1: Review of risk factors related to Adult ADHD.
Discussion and Conclusion
The
data obtained from the present study show the prevalence of Adult ADHD in
psychiatric clinic outpatients at 39.3%. The prevalence rate obtained in the
present study is higher than in similar studies. In a study conducted by
Valsecchi et al. on Italian psychiatric outpatients, the overall prevalence of
adult ADHD was reported as 6.9% (24). In order to evaluate patients with Adult
ADHD, they subjected the patients who were diagnosed with Adult ADHD in the
ASRS-V1.1 questionnaire to a specialized interview. So, patients were screened
more intensively than using a questionnaire alone.
In
other community-based studies, the observed prevalence is lower than in the
present study. Polyzoi et al., and 2018 (26) On a Swedish population, the
prevalence rate in people aged 18 years and older was estimated to be 3.54 per
1000 people. Vňuková et al., in 2021 (23). In the Czech Republic, the
prevalence of Adult ADHD was assessed as 7.84% based on the 6-item ASRS
questionnaire. On the other hand, the 6-item ASRS questionnaire shows that the
reported rate is lower than the actual level (27), for this reason, the
predicted prevalence in this study was evaluated as 14%. De Zwaan et al., in
2012, the raw prevalence rate of ADHD was evaluated as 4.7% (28).
Ghoreishizadeh et al., in 2014, the prevalence rate in adults aged 18-45 years
was evaluated as 3.8% (29).
The
relatively high prevalence of observation in the present study can have various
reasons. The people who entered the study were selected as available and from
the population with psychiatric disorders. On the other hand, in a random
sample of people who have a psychiatric illness, they may have a high
percentage of Adult ADHD. According to the studies, Adult ADHD can be
associated with other psychiatric diseases such as substance use disorder, mood
disorders (such as depression and bipolar disorder) and anxiety disorders. ADHD
and dysthymic disorder/depression are commonly associated, and the prevalence
of depression in individuals with ADHD varies from 18.6% to 53.3% in different
studies (30, 31). Similarly, studies have reported comorbid ADHD in individuals
with depression at rates of 9% to 16% (32), with an average incidence of 7.8% (33).
The risk of anxiety disorders in people with ADHD is higher than in the general
population, approaching 50% (28). Probably the most common comorbidity with
ADHD is substance use disorder (SUD), especially alcohol or nicotine, cannabis,
and cocaine (34).
Reports
indicate that personality disorders are present in more than 50% of adults with
Adult ADHD, usually cluster B and C personality disorders, and 25% of
individuals have two or more personality disorders (35).
Also,
there are studies showing the relationship between ADHD and bipolar disorder (36),
sleep disorders (21), obesity (37), Internet addiction, virtual networks and
video games (38). In other studies that have been conducted on adults with
Adult ADHD, the age limit was 18 years and above, which also included the
elderly, based on previous studies, with increasing age, especially in old age,
the rate of adult ADHD decreases, while in the present study, the upper age
limit of the people who entered the study was 45 years. Also, the average age
of the people included in the present study was lower compared to the reviewed
studies (20,21,39). The error in the answer should also be taken into account.
In
the present study, the prevalence of adult ADHD was not statistically related
to the age of the subjects. While in the study of Valsecchi et al., (24) in
2021, people with Adult ADHD were younger than people without Adult ADHD. Also,
in a study, De zwaan et al. reported a decrease in the prevalence of ADHD with
increasing age. However, De Zwaan et al., (29) observed a significant
difference between the age groups of 18 to 24 years and 55 to 64 years, while
the other age groups did not have a significant difference, which is similar to
the age group of present study (28).
In
the present study, there was no correlation between the prevalence of adult
ADHD and gender. There is evidence that shows that the rate of ADHD in boys is
2 to 3 times higher than that of girls, but in adults, this ratio tends to
equalize in the studies conducted (24). Also, in the study of Polyzoi et al.,
similar findings were observed with the present study, and no difference was
observed in the incidence of Adult ADHD between men and women (26). On the
other hand, a study conducted by Zetterqvist et al., (24) showed a higher
prevalence in adult men. Because Zetterqvist's study was conducted between 2006
and 2009, it can be concluded that the proportion of women with adult ADHD has
increased over time.
However,
these results do not mean that the graduate education level is a protective
factor against Adult ADHD. Various studies show a moderate association between
IQ and attention deficits (40), and the diagnosis of ADHD has the same validity
among children with high IQ and children with average IQ. It can be concluded
that people diagnosed with Adult ADHD who have a high level of education
compensate for their functional deficit due to ADHD with a lower IQ compared to
their peers.
In
the present study, a significant relationship between drug use and adult ADHD
was observed, and 56.9% of people who use drugs have adult ADHD. This finding
is expected, as ADHD is typically associated with risky behaviors and
decision-making problems (41). The present finding has also been shown in
various studies (24, 28, 42) In descriptive reports and demographic studies,
adult ADHD patients have described marijuana as helpful in controlling
inattention and impulsivity (43, 44). In a study conducted by Notzon et al.
(45), the prevalence of marijuana use was estimated at 34-46%. ROMO et al. also
observed a higher rate of marijuana use, alcohol use, and gambling in people
with Adult ADHD (46).
In
examining the relationship between marital status and adult ADHD, our findings
did not show a significant relationship, which is consistent with the
observations of Valsecchi et al. (24). But they observed that most people with
Adult ADHD are single and less likely to have a partner. In some previous
studies, no significant relationship between marital status and adult ADHD has
been observed (2, 13, 29). Some studies show that the prevalence of Adult ADHD
is higher in divorced people (15, 47). Also, in another study, the prevalence
of Adult ADHD was higher in widowed, divorced and single people (48). But,
considering the effect of Adult ADHD in adults and in their intimate
relationships, which leads to less stability and higher divorce rates, judging
the impact of this disorder on marital status may require longer follow-ups. In
the investigation of being employed, no significant relationship between being
employed and Adult ADHD was observed, as some studies had similar results (24,
28). While other studies have shown a higher prevalence of Adult ADHD in
unemployed people (15, 48).
The
main limitation of the present study is the absence of a secondary follow-up
for the additional examination of people who are diagnosed with Adult ADHD in
the ASRS-v1.1 questionnaire due to the COVID-19 pandemic and quarantine
restrictions, as well as the lack of cooperation of the patients in the
circumstances. Considering the high prevalence that was observed, maybe a more
detailed investigation by dedicated interviews could have brought us more
accurate results. For example, Valsecchi et al. (24) subjected patients who
scored above 50 in the ASRS-v1.1 questionnaire to a dedicated DIVA interview.
The next limitation is the insufficient sample size, which may have caused the
variables related to Adult ADHD to not be evaluated correctly. On the other hand,
we did not have any information about the underlying disease and the history of
ADHD or ADHD symptoms in the childhood of these people. The findings of the
present study show that the prevalence of Adult ADHD is high among patients who
refer to the Babol Psychiatric Clinic as an outpatient. This shows the
importance of using appropriate screening methods in these people, early
diagnosis and treatment. Also, people who have a history of using tobacco
and/or alcohol and/or especially drugs, or are currently using them, should be
screened for Adult ADHD so that we can prevent more problems for them with
early diagnosis.
Authors contributions
SJ conceived and
designed the analysis, SMZ collected the data, MA contributed
data or analysis tools, HGh wrote the paper, AM performed the
analysis.
References
1.
Kaisari P., Dourish C.T.,
Higgs S. Attention Deficit Hyperactivity Disorder (ADHD) and disordered eating
behaviour: A systematic review and a framework for future research. Clinical
psychology review, 2017; 53:109-21.
2.
De Graaf R., Kessler R.C.,
Fayyad J., Ten H. M., Alonso J., Angermeyer M. The prevalence and effects of
adult attention-deficit/hyperactivity disorder (ADHD) on the performance of
workers: results from the WHO World Mental Health Survey Initiative. Occupational
and environmental medicine, 2008; 65(12):835-42.
3.
Amira H., Mohammed Hala A.,
Abdel G., Ahmed M.M.M. Gross motor development in Egyptian preschool children
with attention deficit hyperactivity disorder: Pilot study. Journal of Advanced
Pharmacy Education & Research, 2017; 7(4): 438- 442.
4.
Barkley, R. A. Executive
functions: What they are, how they work, and why they evolved. The Guilford
Press; 2012.
5.
Barkley R.A., Fischer M.,
Smallish L., Fletcher K. Young adult outcome of hyperactive children: adaptive
functioning in major life activities. Journal of the American academy of child
& adolescent psychiatry. 2006; 45(2):192-202.
6.
Barkley R.A., Cox D. A
review of driving risks and impairments associated with
attention-deficit/hyperactivity disorder and the effects of stimulant
medication on driving performance. Journal of safety research. 2007;
38(1):113-28.
7.
Dalsgaard S, Østergaard SD,
Leckman JF, Mortensen PB, Pedersen MG. Mortality in children, adolescents, and
adults with attention deficit hyperactivity disorder: a nationwide cohort
study. The Lancet. 2015;385(9983):2190-6.
8.
Polanczyk G., Maurício
S.L., Bernardo L. H., Joseph B., Luis A. R. The Worldwide Prevalence of ADHD: A
Systematic Review and Metaregression Analysis. American Journal of Psychiatry,
2007;164(6):942-8.
9.
Simon V., Czobor P., Bálint
S., Mészáros A., Bitter I. Prevalence and correlates of adult attention-deficit
hyperactivity disorder: meta-analysis. The British Journal of Psychiatry.
2009;194(3):204-11.
10.
Faraone S.V., Biederman J.,
Mick E. The age-dependent decline of attention deficit hyperactivity disorder:
a meta-analysis of follow-up studies. Psychological medicine, 2006;
36(2):159-65.
11.
Polanczyk G., Caspi A.,
Houts R., Kollins S.H., Rohde L.A., Moffitt T.E. Implications of extending the
ADHD age-of-onset criterion to age 12: results from a prospectively studied
birth cohort. Journal of the American Academy of Child & Adolescent Psychiatry,
2010; 49(3):210-6.
12.
Matte B., Anselmi L., Salum
G., Kieling C., Gonçalves H., Menezes A. ADHD in DSM-5: a field trial in a
large, representative sample of 18-to 19-year-old adults. Psychological
medicine. 2015; 45 (2):361-73.
13.
Fayyad J., De Graaf R.,
Kessler R., Alonso J., Angermeyer M., Demyttenaere K. Cross-national prevalence
and correlates of adult attention-deficit hyperactivity disorder. The British
Journal of Psychiatry, 2007;190(5):402-9.
14.
Fischer A.G., Bau C.H.,
Grevet E.H., Salgado C.A., Victor M.M., Kalil K.L.. The role of comorbid major
depressive disorder in the clinical presentation of adult ADHD. Journal of
psychiatric research, 2007;41(12):991-6.
15.
Kessler R.C., Adler L.,
Barkley R., Biederman J., Conners C.K., Demler O. The prevalence and correlates
of adult ADHD in the United States: results from the National Comorbidity
Survey Replication. American Journal of psychiatry, 2006; 163(4):716-23.
16.
Tamam L., Karakus G.,
Ozpoyraz N. Comorbidity of adult attention-deficit hyperactivity disorder and
bipolar disorder: prevalence and clinical correlates. European archives of
psychiatry and clinical neuroscience, 2008; 258:385-93.
17.
Ohlmeier M.D., Peters K.,
Kordon A., Seifert J., Wildt B.T., Wiese B. Nicotine and alcohol dependence in
patients with comorbid attention-deficit/hyperactivity disorder (ADHD). Alcohol
& Alcoholism, 2007; 42(6):539-43.
18.
Dom G., Moggi F.
Co-occurring addictive and psychiatric disorders: Springer; 2016.
19.
Groenman A.P., Oosterlaan
J., Rommelse N.N., Franke B., Greven C.U., Hoekstra P.J.Stimulant treatment for
attention-deficit hyperactivity disorder and risk of developing substance use
disorder. The British Journal of Psychiatry, 2013;203(2):112-9.
20.
Silva D., Houghton S.,
Hagemann E., Jacoby P., Jongeling B., Bower C. Child attention deficit
hyperactive disorder co morbidities on family stress: effect of medication.
Community mental health journal, 2015;51:347-53.
21.
Cortese S., Faraone S.V.,
Konofal E., Lecendreux M. Sleep in children with
attention-deficit/hyperactivity disorder: meta-analysis of subjective and
objective studies. Journal of the American Academy of Child & Adolescent
Psychiatry, 2009; 48(9):894-908.
22.
Schneider H.E., Lam J.C.,
Mahone E.M. Sleep disturbance and neuropsychological function in young children
with ADHD. Child Neuropsychology, 2016; 22(4):493-506.
23.
Vňuková M., Ptáček R.,
Děchtěrenko F., Weissenberger S., Ptáčková H., Braaten E. Prevalence of ADHD
symptomatology in adult population in the Czech Republic–A National Study.
Journal of Attention Disorders. 2021; 25(12):1657-64.
24.
Valsecchi P., Nibbio G.,
Rosa J., Tamussi E., Turrina C., Sacchetti E. Adult ADHD: prevalence and
clinical correlates in a sample of Italian psychiatric outpatients. Journal of
Attention Disorders, 2021; 25(4):530-9.
25.
Mokhtari H., Rabiei M.,
Salimi S.H. Psychometric properties of the persian version of adult
attention-deficit/hyperactivity disorder self-report scale. Iranian Journal of
Psychiatry and Clinical Psychology, 2015; 21(3):244-53.
26.
Polyzoi M., Ahnemark E.,
Medin E., Ginsberg Y. Estimated prevalence and incidence of diagnosed ADHD and
health care utilization in adults in Sweden–a longitudinal population-based
register study. Neuropsychiatric disease and treatment, 2018:1149-61.
27.
Kessler RC, Adler LA,
Gruber MJ, Sarawate CA, Spencer T, Van Brunt DL. Validity of the World Health
Organization Adult ADHD Self‐Report Scale (ASRS) Screener in a representative
sample of health plan members. International journal of methods in psychiatric
research, 2007; 16(2):52-65.
28.
De Zwaan M., Gruss B.,
Müller A., Graap H., Martin A., Glaesmer H. The estimated prevalence and
correlates of adult ADHD in a German community sample. Eur Arch Psychiatry Clin
Neurosci, 2012; 262(1):79-86.
29.
Amiri S., Ghoreishizadeh
M.A., Sadeghi-Bazargani H., Jonggoo M., Golmirzaei J., Abdi S. Prevalence of
adult attention deficit hyperactivity disorder (Adult ADHD): tabriz. Iranian
journal of psychiatry, 2014; 9(2):83.
30.
Torgersen T., Gjervan B.,
Rasmussen K. ADHD in adults: a study of clinical characteristics, impairment
and comorbidity. Nordic journal of psychiatry, 2006; 60(1):38-43.
31.
Research APADo. Highlights
of changes from dsm-iv to dsm-5: Somatic symptom and related disorders. Focus,
2013;11(4):525-7.
32.
McIntosh D., Kutcher S.,
Binder C., Levitt A., Fallu A., Rosenbluth M. Adult ADHD and comorbid
depression: a consensus-derived diagnostic algorithm for ADHD. Neuropsychiatric
disease and treatment, 2009:137-50.
33.
Bond D.J., Hadjipavlou G.,
Lam R.W., McIntyre R.S., Beaulieu S., Schaffer A. The Canadian Network for Mood
and Anxiety Treatments (CANMAT) task force recommendations for the management
of patients with mood disorders and comorbid attention-deficit/hyperactivity
disorder. Ann Clin Psychiatry, 2012; 24(1):23-37.
34.
Klassen L., Bilkey T.,
Katzman M., Chokka P. Comorbid attention deficit/hyperactivity disorder and
substance use disorder: treatment considerations. Current drug abuse reviews,
2012; 5(3):190-8.
35.
Olsen J.L., Reimherr F.W.,
Marchant B.K., Wender P.H., Robison R.J. The effect of personality disorder
symptoms on response to treatment with methylphenidate transdermal system in
adults with attention-deficit/hyperactivity disorder. The Primary Care Companion
for CNS Disorders, 2012;14(5):26293.
36.
Michelini G., Kitsune V.,
Vainieri I., Hosang G.M., Brandeis D., Asherson P. Shared and disorder-specific
event-related brain oscillatory markers of attentional dysfunction in ADHD and
bipolar disorder. Brain topography, 2018;31:672-89.
37.
Cortese S., Moreira-Maia
C.R., Fleur D., Morcillo-Peñalver C., Rohde L.A., Faraone S.V. Association
between ADHD and obesity: a systematic review and meta-analysis. American
Journal of psychiatry, 2016;173(1):34-43.
38.
Romo L., Rémond J.J.,
Coeffec A., Kotbagi G., Plantey S., Boz F. Gambling and Attention Deficit
Hyperactivity Disorders (ADHD) in a population of french students. Journal of
Gambling Studies, 2015;31:1261-72.
39.
Sobanski E., Banaschewski
T., Asherson P., Buitelaar J., Chen W., Franke B. Emotional lability in
children and adolescents with attention deficit/hyperactivity disorder (ADHD):
clinical correlates and familial prevalence. Journal of Child Psychology and Psychiatry,
2010; 51(8):915-23.
40.
Jepsen J.R.M., Fagerlund
B., Mortensen E.L. Do attention deficits influence IQ assessment in children
and adolescents with ADHD? Journal of Attention Disorders, 2009;12(6):551-62.
41.
Dekkers T.J., Popma A.,
Rentergem J.A.A., Bexkens A., Huizenga H.M. Risky decision making in
attention-deficit/hyperactivity disorder: A meta-regression analysis. Clinical
psychology review, 2016;45:1-16.
42.
Bachmann C.J., Philipsen
A., Hoffmann F. ADHD in Germany: trends in diagnosis and pharmacotherapy: a
country-wide analysis of health insurance data on
attention-deficit/hyperactivity disorder (ADHD) in children, adolescents and
adults from 2009–2014. Deutsches Ärzteblatt International, 2017;114(9):141.
43.
Loflin M., Earleywine M.,
De Leo J., Hobkirk A. Subtypes of attention deficit-hyperactivity disorder
(ADHD) and cannabis use. Substance use & misuse, 2014;49(4):427-34.
44.
Wilens T.E. Impact of ADHD
and its treatment on substance abuse in adults. Journal of Clinical Psychiatry,
2004;65:38-45.
45.
Notzon D.P., Pavlicova M.,
Glass A., Mariani J.J., Mahony A.L., Brooks D.J. ADHD is highly prevalent in
patients seeking treatment for cannabis use disorders. Journal of attention
disorders, 2020;24(11):1487-92.
46.
Romo L., Ladner J., Kotbagi
G., Morvan Y., Saleh D., Tavolacci M.P. Attention-deficit hyperactivity
disorder and addictions (substance and behavioral): Prevalence and
characteristics in a multicenter study in France. Journal of Behavioral
Addictions, 2018;7(3):743-51.
47.
Sobanski E., Brüggemann D.,
Alm B., Kern S., Deschner M., Schubert T. Psychiatric comorbidity and
functional impairment in a clinically referred sample of adults with
attention-deficit/hyperactivity disorder (ADHD). European archives of
psychiatry and clinical neuroscience, 2007;257:371-7.
48.
Park S., Cho M.J., Chang
S.M., Jeon H.J., Cho S.J., Kim B.S. Prevalence, correlates, and comorbidities
of adult ADHD symptoms in Korea: results of the Korean epidemiologic catchment
area study. Psychiatry Res, 2011;186(2-3):378-83.
![]() (1)
(1)