Malignant
transformation of multiple exostosis: a case report
Birundha B 1 *, Senthil Kumaran 1, Jeya Shambavi
1
1 Department of Pathology, Aarupadai Veedu Medical College and Hospital, Vinayaka
Mission's Research Foundation (Deemed to be University), Pondicherry, India
Corresponding Authors: Birundha B
* Email: bvbrindha693@gmail.com
Abstract
Introduction: Osteochondroma is a benign tumor of bone. Malignant transformation of Osteochondroma
is the most devastating complication one can encounter. Osteochondroma can
transform into any malignancy like Osteosarcoma, Chondrosarcoma and Ewing
sarcoma. Malignant transformation is more common in patients with multiple
exostosis. Recognition of this malignant transformation is needed to predict
the patient's outcome.
Case presentation: A 26-year-old male patient came with complaints of a mass in the
left knee region for the past 7 years. X-ray of the knee showed multiple
pedunculated exostosis on either side of the distal end of the femur, tibia and
fibula. Histopathological examination revealed a bony lesion with a
cartilaginous cap of increased thickness and cellularity. The cartilaginous cap
possesses plump chondrocytes showing binucleation-forming nodules with mild
atypia. The cartilaginous cap undergoes endochondral ossification, suggesting
the possibility of a secondary peripheral atypical cartilaginous tumor from
osteochondroma of the tibia.
Discussion: Chondrosarcoma is a heterogeneous type of primary bone cartilaginous
malignancy with variable clinical outcomes. Malignant transformation of
osteochondroma in the appendicular skeleton was named atypical cartilaginous
tumor; in the axial skeleton, it is named Grade 1 Chondrosarcoma.
Conclusion: Differentiation between osteochondroma and its malignant transformation
can be possible if made in a multidisciplinary setting such as clinical
history, radiological findings along with histology to confirm the diagnosis.
Keywords: Osteochondroma, Chondrosarcoma, Bone tumour
Introduction
Osteochondroma the most common benign tumour of bone
accounts for about 35% of benign bone tumours affecting 3% of the population
(1-3). Osteochondroma arises from the metaphysis of bones most commonly in the
second to third decade of life. Commonly affected bones are long bones of the
leg, scapula and pelvis (4).
Osteochondroma
usually presents as a painless, asymptomatic mass and is usually found as an
incidental finding. Osteochondroma are benign cartilage forming tumor derived
from aberrant cartilage of the perichondral ring that may present either as
solitary osteochondroma or multiple hereditary exostosis leading to syndromic
manifestation of the lesion (5,6).
Osteochondromas
are mostly treated by surgical excision of the lesion either partially or
completely. The most common complication of osteochondroma is its malignant
transformation. Osteochondroma can transform into osteosarcoma, chondrosarcoma
and Ewing sarcoma (7,8). Malignant transformation of osteochondroma into
chondrosarcoma is considered as drastic complication of osteochondroma
accounting for about less than 1% of the cases (9). 3-5% of patients with
multiple osteochondromas undergo malignant transformation (10). Here we present
a case of a young male with multiple exostosis presenting with malignant
transformation.
Case presentation
A
26-year-old male patient came with complaints of pain in the left knee for the
past 7 years. The patient took medications for 3-4 years as analgesics, but
after 4yrs since patient was suffering from more pain and swelling over the
knee joint, he took X-ray, X-ray showed mass in the left knee region. History
of pain during rest and walking. The swelling was insidious in onset,
progressive in nature, not mobile, hard in consistency, fixed to the underlying
bone. No history of any previous surgery or chemo or radiotherapy.
The
patient had undergone radiological examination and X-ray knee showed multiple
pedunculated exostosis noted on either side of distal end of femur, Proximal
end of tibia and fibula
(Figure 1).

Figure
1.
Xray image of the patient showing lobulated mass over tibia and fibula.
Reconstructed
3D imaging showed multiple sessile and pedunculated exostosis noted in multiple
visualized bones, largest measuring 6.2 x 6.2 x 6.6cm. Pedunculated
metaphyseal exostosis away from joint space in the medial aspect of proximal
tibia with calcification of chondroid matrix, suggesting the possibility of
Osteochondroma with sarcomatous transformation. (Figure 2). There is no
significant family history of any bone lesions.

Figure
2. Reconstructed
3D image of the patient showing multiple pedunculated mass over the tibia and
fibula.
Excision
of a single pedunculated mass from the lateral aspect of tibia was received
which showed a single bony tissue with a cartilaginous cap totally measuring 6
x 3.5 x 4 cm. Cut surface shows bone tissue measuring 3.5 x 2.5cm with
irregular nodular cartilage cap of varying thickness measuring 2.5cm at its
thickest portion permeating into the bony stalk (Figure 3).

Figure
3. Bony
stalk with cartilaginous cap of varying thickness and permeation into the bone.
Histopathological examination revealed a bony lesion with
cartilaginous cap of increased thickness and cellularity. Cartilaginous
cap increased cellularity possess plump chondrocytes showing
binucleation forming nodules with mild nuclear enlargement, irregularity and
atypia. Cartilaginous cap undergoes endochondral ossification
as in a case of osteochondroma, suggesting the possibility of Secondary
peripheral atypical cartilaginous tumor from osteochondroma of tibia (Figure
4,5).

Figure
4. Histopathological
image showing cartilage undergoing endochondral osssification
(H&E stain, 10X).
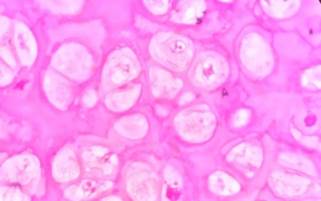
Figure
5. Histopathological
image showing nodules of chondrocytes exhibiting mild atypia (H&E stain,
40X).
Discussion
Hereditary multiple osteochondromas (HMO), an autosomal
dominant disorder involves two or more exostoses in the axial or appendicular
skeleton. It is diagnosed by presence of two or more osteochondromas, detected
radiographically in the metaphyseal ends of the long bones (11).
Chondrosarcoma is a heterogeneous type of primary bone
cartilaginous malignancy with variable clinical outcomes (12). These are locally aggressive,
hyaline cartilage-producing neoplasm arising within the cartilaginous cap of a
pre-existing osteochondroma, tumours in the
appendicular skeleton can be called as peripheral atypical cartilaginous tumor and tumours of the axial
skeleton (including the pelvis, scapula, and skull base) can be called
peripheral chondrosarcoma Grade 1 (13).
The
incidence of chondrosarcoma varies between various bones with Ileum (19%),
followed by the scapula (15%), pubic bone (10%), ribs (10%), tibia (12%) and femur (11%) (13).
Patients
with multiple osteochondromas carrying germline mutations in EXT1 or EXT2 are at increased
risk of developing ACT/CS1 within the cartilaginous cap of osteochondromas. Malignancy risk in case of multiple osteochondromas is as high as
about 5% when compared to solitary osteochondromas which is about 1% (14).
Functional loss of genes EXT1 and EXT2 encoding
glucosyltransferases which is involved in the synthesis of heparan sulfate causes Hereditary multiple exostosis (HME). HME
genetic transmission occurs in autosomal dominant pattern or loss of
heterozygosity or haploinsuffiency or through
mutations in post- transcriptional regualtory
pathways.
Even isolated mutations of EXT1 and EXT2 gene cause
pathology affecting the patient's growth. Malignant transformation is usually
rare accounting for about 2 to 4% in patients affected by HME. A
well-differentiated carcinoma is usually diagnosed, but very rarely
osteosarcomas and dedifferentiated chondrosarcomas from bone could arise (15).
Differentiation
between osteochondroma and its malignant transformation can be possible if made
in a multidisciplinary setting such as clinical history,
radiological findings along histology to confirm the diagnosis (14).
Treatment
of Multiple exostosis is surgical removal, especially in symptomatic cases
irritating adjacent structures. Though the treatment strategies are limited,
precise diagnosis is essential for management. In Future, molecular analysis of
EXT1 and EXT2 genes is essential for understanding the disease at molecular and
cellular level and reveals new treatment options or therapeutic targets in both
Hereditary multiple exostosis and chondrosarcoma (15).
Chemotherapy
and radiation are not indicated for chondrosarcoma since they are resistant to
both. Grade I chondrosarcoma with minimal rate of metastasis in the extremities
are treated by intralesional curettage, high speed burring and adjuvant
treatment with internal fixation and packing using phenol or ethanol or liquid
nitrogen. Lesions in pelvis or axial skeleton needs wide local excision (15).
The
5-year and 10-year local recurrence rates for secondary peripheral
chondrosarcoma are 15.9% and 17.5% respectively. The
5-year and 10-year mortality rates are 1.6% and 4.8% respectively. Local
recurrences are possible due to incomplete excision in inaccessible locations
(14).
Conclusion
This
case report deals with the most common bone tumour
osteochondroma undergoing malignnat transformation
which emphasize the fact that multiple disciplinary evaluation, as well as
careful gross examination, helps us to make the proper diagnosis at the
appropriate time which helps in improving the prognosis and outcome of the
patient.
We hope that this case report raises awareness among
clinicians and pathologists to this possible transformation of osteochondroma
to chondrosarcoma, and that thorough investigation drives further development
in the diagnosis and safe treatment for improving patient outcomes.
Author
contribution
BB: Conceptualization, Data curation, Formal analysis, Investigation,
Methodology, Project administration, Resources, Software, Supervision,
Validation, Visualization, Writing original draft. SK:
Conceptualization, Data curation, Formal analysis, Funding acquisition,
Investigation, Methodology, Project administration, Resources, Visualization,
Writing original draft. JS: Conceptualization, Data curation, Formal
analysis, Funding acquisition, Investigation, Methodology, Project
administration, Resources, Software, Supervision, Validation, Visualization, Writing original draft, Writing review & editing
Conflict
of interest
The
authors declare that they have no competing interests.
Funding
There
is no funding agency involved in this research.
References
1. Kitsoulis P, Galani V, Stefanaki K, et al. Osteochondromas: review of the
clinical, radiological and pathological features. In Vivo. 2008;22(5):633-46.
2. Morton KS. On the question of recurrence of
osteochondroma. J Bone Joint Surg Br.
1964;46(4):723-5.
3. Saglik Y, Altay M, Unal
VS, Basarir K, Yildiz Y. Manifestations and
management of osteochondromas: a retrospective analysis of 382 patients. Acta Orthop Belg. 2006;72(6):748- 55.
4. Tianjun Lan, Xin Liu, Pei-Sheng Liang,Qian Tao. Osteochondroma of coronoid process: A
case report send review of literature. Oncol Lett.2019;18:2270-2277.
5. Vikram V Kadu, Saindane
KA, Ninad Goghate, Neha Goghate.
Osteochondroma of the Rib: A rare radiological appearance. J Orthop Case Rep. 2015;5:62- 64.
6. Dr. Gyneshwar
Tank, Dr. Sumit Agarwal, Dr.
Kalom Jamoh. Osteochondroma transform into secondary low-grade
chondrosarcoma with similar histology features: Case report. Int J Case Rep Orthop 2022;4(2):09.
7. Moradi Tabriz H, Obohat M, Vahedifard
F, Eftekharjavadi A. Survey of Mast Cell Density in
Transitional Cell Carcinoma. Iran J Pathol.
2021;16(2):119-27.
8. Salari S, Ghadyani M, Karimi M, Mortezazadeh
M, Vahedifard F. Immunohistochemical Expression
Pattern of MLH1, MSH2, MSH6, and PMS2 in Tumor
Specimen of Iranian Gastric Carcinoma Patients. Journal of Gastrointestinal
Cancer. 2022;53(1):192-6:10.
9. Kuruwitaarachchi, Kasun & Munidasa,
Dilshan.Secondary chondrosarcoma from a solitary
osteochondroma of the fibula head: a case report. Journal of the Postgraduate
Institute of Medicine.2021.8:135.
10.
Tsuda, Yusuke & Gregory, Jonathan & Fujiwara, Tomohiro & Abudu, Seggy. Secondary chondrosarcoma arising from
osteochondroma: outcomes and prognostic factors. The bone & joint journal.
2019:101-B. 1313-1320.
11. Vlok SCS, Wagener GWW, Zaharie D. Secondary
chondrosarcoma: Malignant transformation of pre-existing hereditary and
nonhereditary cartilaginous lesions. S Afr J Rad.
2014;18.
12. Arsenault M, Alam W, Lambert T, Li S, Adorno DN,
et al. Secondary Chondrosarcoma Arising from Osteochondroma: Case Report and
Literature Review. JSM Clin Cytol Pathol 2019: 4:3.
13. Sbaraglia M, Bellan E,
Dei Tos AP. The 2020 WHO Classification of Soft
Tissue Tumours: news and perspectives. Pathologica.
2021 Apr;113(2):70-84.
14.
Goldblum JR, Lamps LW, Mckenney JK, Myers JL, Rosai
J. Rosai and Ackerman’s Surgical Pathology. Philadelphia, Pa: Elsevier; 2018.
15. Ottesen TD, Shultz BN, Munger AM, Amick M, Toombs CS, Friedaender GE, Grauer JN. Chondrosarcoma patient
characteristics, management, and outcomes based on over 5,000 cases from the
National Cancer Database (NCDB). PLoS One. 2022 Jul
28;17(7):e0268215.