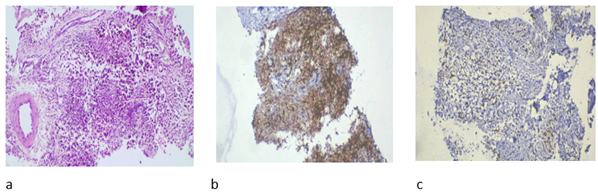
Figure 1. a: high power view showing epithelioid
cells and spindle cells along with congested vessels, b: Immunohistochemistry
showing diffuse positivity for CD68, c: Immunohistochemistry showing focal
positivity for desmin.
Recurrent diffuse tenosynovial
giant cell tumour of knee joint with emphasis on
treatment trends: a case report
Siddharth Arora
1*, Sandeep Ramawat 1, Kriti
Grover 1, Shilpi Singh 1
1 Rohilkhand Medical College and Hospital, Bareilly, Uttar Pradesh,
India
Corresponding
Authors: Siddharth Arora
*
Email: drsiddhartharora25@gmail.com
Abstract
Introduction: Tenosynovial giant cell tumor is
a benign lesion that frequently recurs locally. The recurrence rate is quite
high for diffuse tenosynovial giant cells. Complete
surgical excision remains the standard of treatment, yet radiotherapy can be
delivered in cases of recurrence. Here we present a case of recurrent diffuse tenosynovial giant cell treated with Image Guided-Intensity
modulated radiotherapy. The case report also highlights and discusses other
potential treatment options available or under investigation.
Case presentation: A 32-year-old female presented to us as a recurrent case of Diffuse tenosynovial giant cell tumor (DTGCT). She was
offered above-knee amputation, which she refused. The role of systemic therapy
was explored. She was taken for Image-guided; intensity-modulated radiotherapy
(IG-IMRT).
Discussion: DTGCT shows a widespread morphological spectrum. Though Surgery
remains the standard of care, Post op radiotherapy can be delivered in
incomplete synovectomy or recurrence cases. The potential use of agents
targeting CSF1/ CSF1R in D-TGCT has been explored.
Conclusion: Post operative radiotherapy with advanced External beam radiation
therapy techniques IG-IMRT, after surgery produced acceptable functional status
and excellent local control with few side effects. Our patient post
radiotherapy phase was uneventful. His 6-month evaluation was suggestive of no
recurrence.
Keywords: Tenosynovial giant cell tumor, Surgery,
Radiotherapy
Introduction
Tenosynovial giant cell tumor is a soft tissue tumor classified by WHO into localised-type (L-TGCT) and diffuse-type (D-TGCT). L- TGCT
is more common than D-TGCT. Most patients present with complaints of swelling
around the joints and restriction of movements associated with pain (1). MRI
helps establish D-TGCT diagnosis. It also serves as a choice to assess residual
D-TGCT after synovectomy and for postoperative follow-up. The standard
treatment of choice is surgery, but an adjuvant radiotherapy option can be
considered in recurrent cases or as a post-operative adjuvant in residual
cases. Recurrences can reach as high as upto 60% for
D-TGCT, whereas they are as low as 4 % in case of L-TGCT. Microscopic
characteristics include lipid-rich macrophages, large cells, hemosiderin
deposits, and fibrous stroma. Due to its locally aggressive character, PVNS can
cause osteoarthritis and joint destruction if left untreated. Image-guided
approach (IGRT) Intensity-modulated radiation treatment has shown notable
clinical benefits, including improved response and less toxicity to the
surrounding normal tissues (2,3). For D-TGCT, the potential use of agents
targeting CSF1/ CSF1R in D-TGCT has been explored (4,5). Here we present a
recurrent case of D-TGCT in a middle-aged female who under adjuvant radiotherapy
using Image guidance. Here we report a case of recurrent Diffuse tenosynovial giant cell tumor post multiple surgeries,
treated with advanced radiotherapy technique. Other possible treatment options
that are available or being investigated are also highlighted and discussed in
the case report.
Case
presentation
A 32-year-old female presented initially in 2015
elsewhere with swelling in the anterior aspect of her left knee with no history
of trauma. She underwent surgery and the post-operative histopathological
report was suggestive of Villonodular Synovitis. MRI of the left knee revealed
extensive mass like synovial thickening within the suprapatellar fossa, paracondylar region, popliteal fossa and intrameniscal surface with cortical erosion of fibula,
distal femur and proximal tibia. Features were suggestive of a giant cell
tumor. Synovial Biopsy of my left knee was in favor of a Benign Giant Cell
Tumor-rich lesion. She was offered open arthrotomy with synovectomy of her left
knee with exploration of posteromedial knee in view of varicose veins.
She continued her follow-up with a local practitioner. Now she has
presented to us after nine years with a suspected recurrence. The MRI outside
was suggestive of an ill-defined mass like synovial proliferation in the
patella femoral and tibia femoral joints, which appears hypointense on T1 and
hyperintense on T2/STIR images. The findings represent features of pigmented
villonodular synovitis or diffused synovial Giant Cell tumor. She underwent
core biopsy from swelling of her knee. Histopathological impressions revealed Epithelioid
neoplasm. Immunohistochemistry (IHC) was performed for final confirmation. The
lesion was weak positive for Pan CK, focal positive of p16, Desmin and p63 and
showed diffuse positivity for CD68 (Figure 1).
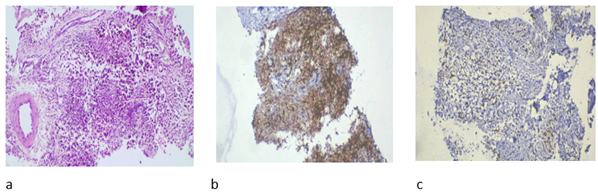
Figure 1. a: high power view showing epithelioid
cells and spindle cells along with congested vessels, b: Immunohistochemistry
showing diffuse positivity for CD68, c: Immunohistochemistry showing focal
positivity for desmin.
The lesion was negative for S100, HMB 45, Melan A,
CD34, CD138, CD45, SAT B2 and MDM2. The final impression with the above IHC was
favorable for diffuse tenosynovial Giant Cell Tumor.
She was offered above-knee amputation, which she refused. The role of
systemic therapy was explored. She agreed to radiotherapy. She was taken for
Image-guided; intensity modulated radiotherapy (IG-IMRT). She tolerated well
without any significant side effects. Her 6 months evaluation was suggestive of
no recurrence. She is doing well and has been kept on follow up. To reduce the
incidence of lower limb edema, elastic stocking and regular lower limb
physiotherapy has been reinforced. She is planned for repeat the imaging after
6 months.
Discussion
Diffuse
tenosynovial giant cell tumor, formerly known as
pigmented villonodular synovitis, is a rare benign mesenchymal tumor which has
its origin from tendon sheaths or synovial bursa or synovial tissue of large
joints. Knee is the most common joint affected (2). The 2020 WHO Classification
defines it as a locally aggressive neoplasm which rarely metastasizes. (6) With
female predilection, it affects the young population and is common at ages 40
and 50 years.
MRI
T1 weighted, T2 weighted or Fluid restricted sequences help to detect residual
DTGCT post synovectomy. A modification of RECIST (m-RECIST) can be applied for
higher accuracy.
For
the detection of hemosiderin associated with tumor bleeding, a gradient-echo
sequence can be useful. Intravenous gadolinium contrast is useful for
post-synovectomy follow-up and for detecting tumors. Bleeding is a common
feature of D-TGCT imaging, and it is typically identified as blooming on
gradient echo images. The severity of D-TGCT is determined by a number of
criteria, including muscle/tendinous, ligament, neurovascular, cartilage
invasion and cortical bone erosion.
Suspicious
DTGCT should be confirmed with the help of image-guided biopsy. Core biopsy,
generally performed under local anesthesia as either CT-guided or USG-guided,
can obtain a representative sample. DTGCT shows a widespread morphological
spectrum. D-TGCT may present as synovial thickening, is characterized as
frond-like with villous or nodular shape. Villous pattern is often exhibited
when intra-articular, whereas tumors show infiltrative margins with
multinodular growth when extra articular. Diffuse-type TGCT (D-TGCT) consists
mostly of mononuclear cells with few multinucleated giant cells, foamy
histiocytes and hemosiderin deposition. Immunohistochemistry in TGCT reveals
expression of clusterin in the large mononuclear
cell. Immunohistochemistry shows clusterin
expression, desmin positivity in mononuclear cells
and CD68, CD 163 and CD 45 positivity in smaller histiocyte-like cells.
Excision
of diseased synovium is the preferred choice. Performing complete resection is
challenging. Mostly open surgical excision along with synovectomy or
arthroscopic excision is the modality adopted. Though adequate synovectomy may
not be sufficient, relapses have been seen as high as in 44% of cases, with
many occurring within 5 years or within 2 years. Results of 40 patients’
arthroscopic excision of PVNS were evaluated in retrospective research by Jain
et al. This clinical series found that arthroscopic excision works effectively
for both diffuse and localized PVNS, as well as for recurrences. Keyhani et al. employed the Lysholm score and the
International Knee Documentation Committee (IKDC) score throughout a 5-year
follow-up. Heijden et al.'s retrospective examination of 30 patients found that
open synovectomy was superior to arthroscopic synovectomy in terms of quality
of life and functional outcome for TGCT knees.
Studies
have shown that post-operative radiotherapy can be offered in incomplete
synovectomy patients, those who refuse surgery or in inoperable patients. With
the advancement of image guidance, the side effects related to conventional
traditional techniques like two-dimensional conformal radiotherapy (2D-CRT) or
three-dimensional conformal radiotherapy (3DCRT) are significantly lower.
Outcomes, on the other hand, in terms of clinical response, are better with low
toxicity to normal tissues documented (2,3). Postoperative adjuvant external
irradiation is currently a crucial treatment for patients with D-TGCT as
numerous publications have demonstrated, and it can greatly enhance local
control (7, 8). The dosage for postoperative radiation, however, is up for
debate. As of right now, the majority of researchers think that the 36Gy total
dose is safe and effective because it is less than the long-term threshold of
joint fibrosis.
Our
patient was immobilized with the help of VacLoc and 2
clamp orfit. A CT scan was performed 10 cm above to
feet with 2. 5 mm slice thickness. MRI and CT images were fused, gross tumor
volume was delineated and CTV was contoured, sparing 1 cm of normal tissue to
decrease chances of lymphedema and including a whole knee joint cavity with
residual disease. The MRI T2 peritumoral edema was included because of the risk
of harboring microscopic extension of the tumor. The planning target volume
(PTV) included the CTV with a 0.3cm isotropic margin. She was planned for 36Gy
in 18 fractions @ 2 Gy per fraction. Volumetric-based inverse planning
intensity-modulated radiation therapy (IMRT) is used as radiotherapy technique
for generating plan. Daily setups were checked with the help of Cone beam CT
(CBCT). Patients who had adjuvant radiation, particularly EBRT, had a much
lower recurrence rate than those who only had surgery (8). Griffin et al in
their series discussed long-term Outcome of the Treatment of High-Risk Tenosynovial Giant CellTumor/Pigmented
Villonodular Synovitis with Radiotherapy and Surgery. The authors concluded
that the addition of moderate-dose adjuvant radiotherapy provided excellent
local control while maintaining good function with low treatment-related
morbidity (9).
Organ-specific
radiation-induced cancer risk estimates due to radiotherapy for benign
pigmented villonodular synovitis discussed by Michalis et al used non-linear
mechanistic model and differential dose-volume histograms obtained by CT-based
3D radiotherapy planning. None of the TGCT-D patients receiving EBRT had early
or late radiation-related problems that were more serious than grade 2,
and none of them developed any cancer induced on by radiation. Commonly
documented side effects are radiation dermatitis, local pain or Lymphedema.
After EBRT, patients have only sometimes had lymphedema, moderate radiation
dermatitis, or local pain, according to a handful of studies.
Radiosynoviorthesis (RSO), usually with ytrrium90, is an additive treatment option (10).
Yet it requires a specialized delivery system and is an invasive procedure.
Systemic therapy can be offered to symptomatic patients and to those with
functional impairment. CSF1 is highly expressed in all TGCT, providing the
basis for targeting the CSF1R pathway expressed by macrophages (4,5). Pexidartinib is an oral selective small molecule inhibitor
that targets colony stimulating factor. It is the first FDA-approved agent in
symptomatic patients (11,12). The ENLIVEN study achieved its endpoint by
comparing the overall response rate for pexidartinib
to the placebo. As a consequence of the enclosed warning about the possibility
of severe and perhaps lethal liver damage, it is only recommended and
administered under a safety program called the Risk Evaluation and Mitigation
Strategy, which is sponsored by the manufacturer. Multiple other agents,
including Vimseltinib (an oral Tyrosine kinase
inhibitor supported by the MOTION 3 study) are under investigation (Table1).
Conclusion
Post
operative radiotherapy should be often considered in recurrent cases. Low
morbidity, excellent local control while maintaining joint function are
additional advantages. Besides IG-IMRT, Proton therapy, SBRT are promising new
advancements, yet more research is needed. Currently, no recommended follow-up
schedules are proposed for D-TGCT. Follow-up is generally based on new-onset
symptoms with MRI of the affected joint after every 6 – 12 months. Frequent
evaluation can be considered in patients needing systemic therapy. We recommend
3 monthly follow-ups in view of multiple recurrences to evaluate response and
residual disease. One promising treatment strategy for TGCT is to target
the CSF1/CSF1R axis.
Inhibitors of CSF1/CSF1R enhance tumor response and alleviate symptoms.
Table
1. Drugs
under investigation and their side effects.
|
M.O. A |
Study |
Side effects |
|
|
Pexidartinib |
oral selective small molecule inhibitor that targets colony
stimulating factor |
Tap et al (13) Phase3, double blind, placebo controlled, RCT |
Primary endpoint: ORR at week 25, based
on blinded central MRI 39% Pexidartinib
vs 0 % placebo Side effects seen with Pexidartinib: hair color
change, fatigue, AST/ALT increase |
|
Imatinib mesylate |
a tyrosine
kinase inhibitor that blocks the driver mechanism of DTGCT in CSF1R |
Verspoor et al (14): Retrospective cohort Locally
advanced, recurrent, or metastatic diffuse TGCT in knee |
Median PFS:18 months Side effects
seen fatigue, edema/fluid retention, nausea, skin rash/dermatitis |
|
Nilotinib |
potent inhibition of CSF1R |
Gelderblom et al (15): Phase 2 trial |
Primary endpoint: proportion of pts progression free at 12wk |
|
Emactuzumab |
a humanized monoclonal antibody targeting CSF1R |
Cassier et al: Phase1trial |
Primary objective: evaluate safety and tolerability,
determine Maximum tolerated dose or Optimal biological dose Common
Adverse effects: facial edema, asthenia, pruritus |
Author
contribution
SA and KG wrote
the main script, revised the script, conceptualized, and prepared figures.
SA gathered resources
Conflict
of interest
There
are no Conflicts of interest.
Funding
There
is no funding.
References
1. Gelhorn HL, Tong S,
McQuarrie K et al (2016) Patient-reported symptoms of tenosynovial
giant cell tumors. Clin Ther 38(4):778–793
2. Joshi K, Huang B, Scanga L, et
al.. Postoperative radiotherapy for diffuse pigmented villonodular
synovitis of the temporomandibular joint. Am J Otolaryngol
2015;36:106–13.
3. Park G, Kim YS, Kim JH, et al..
Low-dose external beam radiotherapy as a postoperative treatment for patients
with diffuse pigmented villonodular synovitis of the knee. Acta Orthopaedica 2012;83:256–60
4. Cupp JS, Miller MA, Montgomery KD, et al.
Translocation and expression of CSF1 in pigmented villonodular synovitis, tenosynovial giant cell tumour, rheumatoid arthtritis and other reactive synovitis. Am J Surg Pathol 2007;31:970–6.
5. Brahmi M, Alberti L, Tirode
F, et al. Complete response to CSF1R inhibitor in a translocation variant of teno-synovial giant cell tumor
without genomic alteration of the CSF1 gene. Ann Oncol 2018;29:1488–9.
6. Righi A, Gambarotti M, Sbaraglia M, et al. Metastasizing tenosynovial
giant cell tumour, diffuse type/pigmented villonodular synovitis. Clin Sarcoma
Res 2015;5: 15.
7. Li
W, Sun X, Lin J, et al. Arthroscopic synovectomy and postoperative assisted
radiotherapy for treating diffuse pigmented villonodular synovitis of the knee:
an observational retrospective study. Pak J Med Sci 2015;31:956–60.
8.
Park G, Kim YS, KimJH, etal.
Low-dose external beam radiotherapy as a postoperative treatment for patients
with diffuse pigmented villonodular synovitis of the knee. Acta Orthopaedica 2012;83:256–60.
9.
Griffin AM, Ferguson PC, Catton CN, et al. Long-term outcome of the treatment
of high-risk tenosynovial giant cell tumor/pigmented villo nodular synovitis with radiotherapy and surgery.
Cancer 2012;118: 4901–9.
10.
Dürr HR, Capellen CF, Klein A, et al: The effects of radiosynoviorthesis
in pigmented villonodular synovitis of the knee. Arch Orthop
Trauma Surg 2019;139:623-627.
11.
Lamb YN. Pexidartinib: First Approval. Drugs. 2019
Nov;79(16):1805-1812. doi:
10.1007/s40265-019-01210-0. Erratum in: Drugs. 2020 Mar;80(4):447. doi: 10.1007/s40265-020-01280-5.
12.
Lewis JH, Gelderblom H, van de Sande M, et al. Pexidartinib long-term hepatic safety profile in patients
with tenosynovial giant cell tumors. Oncologist
2021;26: e863–73.
13.
Tap WD, Gelderblom H, Palmerini E, et al: Pexidartinib versus placebo for advanced tenosynovial giant cell tumour
(ENLIVEN): A randomised phase 3 trial. Lancet 2019;
394:478-487.
14. Verspoor FGM, Mastboom MJL, Hannink G, et al: Long-term efficacy of imatinib mesylate
in patients with advanced tenosynovial giant cell
tumor. Sci Rep 2019;9:14551.
15. GelderblomH, Cropet C, Chevreau C, et al: Nilotinib in locally advanced pigmented
villonodular synovitis: A multicentre, openlabel, single-arm, phase 2 trial. Lancet Oncol 2018;19:639-648.