Decidual cell
aggregates occurring outside the endometrium are termed “ectopic decidua” or
“deciduosis,” a phenomenon first described by Walker in 1887 (1). While
deciduosis most commonly involves the ovaries, uterus, and cervix, localization
in the peritoneum or omentum is distinctly uncommon. These rare sites are
clinically significant because of their potential to mimic malignant or
infectious conditions (2–5).
Ectopic decidua
is generally a benign, self-limiting process, most often associated with
pregnancy and typically regressing postpartum. Nevertheless, its gross and
microscopic appearance can closely resemble serious pathologies such as
peritoneal carcinomatosis, tuberculous peritonitis, or, more rarely, deciduoid
mesothelioma (6,7). Such lesions, when encountered incidentally—particularly
during cesarean section—may be misinterpreted as metastatic disease, leading to
unnecessary concern and investigations.
Histopathological
confirmation remains essential for diagnosis. Omental deciduosis is
characterized by large polygonal cells with abundant eosinophilic cytoplasm and
an absence of significant mitotic activity. Recognition of these features is
crucial to avoid misdiagnosis and to reassure both clinicians and patients.
Recent literature
underscores the importance of heightened awareness among pathologists and
surgeons, as peritoneal and omental deciduosis, though rare, may occur in
reproductive-age women and mimic malignancy both macroscopically and
microscopically (7–9). It should also be emphasized that ectopic deciduosis is
a normal, albeit uncommon, hormonally mediated phenomenon occurring during
pregnancy and generally has no adverse effect on future fertility or the
ability to achieve a successful pregnancy (7).
We present a case
of omental deciduosis in a 29-year-old asymptomatic woman, detected
incidentally during cesarean section. Intraoperatively, multiple nodular
deposits were noted on the omentum, initially raising concern for metastatic
disease. Subsequent histopathological evaluation revealed extensive
decidualization, thereby confirming its benign nature. This case underscores
the clinical significance of recognizing omental deciduosis, as its atypical
presentation and striking resemblance to malignant pathology can create
considerable diagnostic challenges.
Case presentation
A 29-year-old woman, gravida 1 para 0, presented at 36 weeks of
gestation with pregnancy-induced hypertension and signs of fetal distress. She
was admitted for close monitoring and managed with antihypertensive therapy. On
admission, her blood pressure was 160/100 mmHg. Laboratory investigations
revealed elevated liver enzymes (Alanine aminotransferase [ALT] 245 U/L,
Aspartate aminotransferase [AST] 310 U/L) and proteinuria (dipstick 3+),
findings consistent with preeclampsia.
Fetal heart rate monitoring demonstrated persistent non-reassuring
patterns, necessitating an emergency cesarean section. Preoperative
ultrasonography confirmed a viable fetus with reduced amniotic fluid index and
features suggestive of placental insufficiency.
Intraoperatively, multiple small, whitish lesions measuring 1–4 mm were
observed on the peritoneal surfaces of the posterior uterine wall, broad
ligament, ovaries, sigmoid colon, and omentum. A representative omental tissue
specimen was excised and submitted for histopathological examination to exclude
malignancy or other pathological conditions.
Pathological
Findings
The specimen
consisted of a fibrofatty soft tissue fragment measuring 4 × 3 × 2 cm. On gross
examination, multiple discrete whitish nodules, ranging from 1 to 4 mm in
diameter, were scattered throughout the tissue (Figure 1).
Microscopically,
the fibroadipose tissue was composed predominantly of mature adipocytes with
mild chronic inflammatory cell infiltrates. The submesothelial regions revealed
decidual cells arranged singly as well as in small focal nodular clusters.
These cells were large and polygonal, with abundant finely granular
eosinophilic cytoplasm. Their nuclei were round, bland, and contained a single
prominent nucleolus, without atypical features such as pleomorphism,
hyperchromasia, or increased mitotic activity (Figure 2). Importantly, no
epithelioid cell granulomas were identified, thereby excluding granulomatous
inflammation.

Figure 1. Gross image of
peritoneal tissue showing whitish nodules (Black arrow) in the parenchyma.
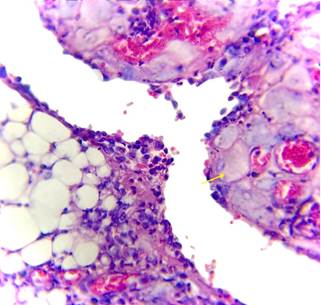
Figure 2. (H&E,
10X)Sections showing decidual tissue invading the peritoneal tissue. A decidual
cells is seen with abundant eosinophilic cytoplasm and round to oval nucleus
and vesicular chromatin (Yellow arrow).
Overall, the
histopathological features were consistent with ectopic decidua (deciduosis),
confirming the benign nature of the nodular deposits and ruling out malignancy
or infectious granulomatous disease.
Discussion
Ectopic decidua,
also termed deciduosis, is most often an incidental microscopic finding
identified during pregnancy-related surgical procedures, such as cesarean
sections, postpartum tubal ligations, appendectomies, or in association with
ectopic tubal pregnancies. The condition is usually asymptomatic and detected
only through histopathological evaluation. In rare instances, however, ectopic
decidua may lead to significant complications, including hemoperitoneum,
pseudo-acute appendicitis, pulmonary involvement, or obstructed labor secondary
to extensive peritoneal deposits (10–13). These uncommon but serious outcomes
highlight the clinical importance of recognizing ectopic decidua, particularly
when lesions are diffuse or symptomatic (14).
The pathogenesis
of ectopic decidua remains incompletely understood, though it is generally
attributed to a heightened hormonal response of endometrial stromal cells to
elevated progesterone levels during pregnancy. Zaystev et al. proposed two main
hypotheses: the more widely accepted mechanism involves progesterone-induced
metaplasia of subcoelomic mesenchymal cells, which typically regress as hormone
levels decline postpartum (15). Alternatively, the de novo development of
decidual cells from peritoneal surfaces has been suggested, though this is less
favored. The hormonal basis of metaplasia accounts for the transient and
self-limiting nature of the condition (16,17).
Histologically,
ectopic decidua can closely resemble malignant processes, making accurate
differential diagnosis essential. Decidual cells may occasionally show mild
atypical features such as hyperchromasia, pleomorphism, or focal hemorrhagic
necrosis, changes that can mimic deciduoid malignant mesothelioma (17). In our
case, the histopathological evaluation demonstrated decidual cells possessing
abundant eosinophilic cytoplasm and round nuclei with prominent nucleoli. The
absence of overt cellular atypia and atypical mitoses supported the benign
nature of the process, leading to the diagnosis of an ectopic decidual
reaction. These features are consistent with previously reported cases and
underscore the importance of distinguishing this benign condition from
malignant mimics.
Immunohistochemistry
(IHC) plays a pivotal role in distinguishing benign deciduosis from malignancy.
Mesotheliomas typically express cytokeratin MNF116, HBME-1, and calretinin,
with epithelial membrane antigen (EMA) showing focal brush border-like positivity,
in contrast to benign decidual cells, which show progesterone receptor (PR) and
CD10 positivity (18,19). Other important differential diagnoses include
metastatic melanoma (positive for S-100 and HMB-45) and signet-ring cell
carcinoma (cytokeratin-positive) (18). Accurate identification is crucial to
prevent unnecessary aggressive management.
Clinically,
ectopic decidual reaction is regarded as a benign, physiological response to
progesterone during pregnancy. Lesions usually regress spontaneously within 4–6
weeks postpartum and do not require specific treatment (8,17). Awareness among
clinicians and pathologists of this entity is therefore essential to avoid
misdiagnosis and overtreatment (20).
In the present
case, the patient responded well to treatment, and follow-up ultrasonography
showed no evidence of recurrence. She has remained disease-free for 18 months
post-surgery, underscoring not only the benign nature of omental deciduosis but
also the importance of accurate diagnosis to prevent unnecessary aggressive
interventions.
Limitation
We acknowledge the absence of frozen section evaluation in this case. We also
emphasize the potential role of immunohistochemistry in better distinguishing
omental deciduosis from its close mimics. However, in the present case, the
diagnosis was confidently established based on clinical presentation and
characteristic histopathological features.
Conclusion
Author contribution
GB concept,
design, literature search, data acquisition, manuscript preparation, manuscript editing and review.
Funding
There
is no funding.
Conflicts
of interest
There
are no conflicts of interest.
References
1. Walker A: Der Bau der
Eihaeute bei Graviditatis abdominalis. Virchows Arch Path Anat 1887, 197:72-99.
2. Heller DS, Skurnick JH.
Ovarian deciduosis mimicking metastatic carcinoma: a case and review of the
literature. Arch Gynecol Obstet. 2011;283(2):381-384.
3. Wong L, Botolahy V,
Carteret T, Marty M, Brun JL. Decidualized ovarian mass mimicking malignancy.
Case Rep Obstet Gynecol. 2015;2015:217367.
4. Charkhchi P, Butcher M,
Macura KJ. Vanishing pelvic mass: Decidualized endometriosis during pregnancy.
Radiol Case Rep. 2024;19(6):2535-2539.
5. Yin M, Wang T, Li S,
Zhang X, Yang J. Decidualized ovarian endometrioma mimicking malignancy in
pregnancy: a case report and literature review. J Ovarian Res. 2022;15(1):33.
6. Zayyan MS, Shittu SO,
Igwegbe AO. Decidualization of the peritoneum in pregnancy: a case report and
review of the literature. Afr Health Sci. 2019;19(3):2469-2474.
7. Elemen L, Akay C,
Gürpinar A, Törüner FB. Deciduosis of the omentum mimicking peritoneal
carcinomatosis. J Pediatr Surg. 2012;47(12):e61-e64.
8. Mandal S, Dhingra KK,
Khurana. Deciduosis of the omentum: a diagnostic dilemma. Indian J Pathol
Microbiol. 2013;56(2):127-128.
9. Cohen S, Bacallao C,
Mealy K. Ectopic decidua of the peritoneum simulating peritoneal
carcinomatosis: report of two cases and review. Int J Surg Pathol.
2018;26(6):517-522.
10. Gupta K, Barya S, Gupta
A, Nikhra P. Ectopic decidual reaction – A diagnostic dilemma [Internet]. IP
Arch Cytol Histopathol Res. 2023 [cited 2025 Sep 22];8(2):116-118.
11. Alhadi A, Youssoufi Y,
Guermazi S. Ectopic deciduosis with gigantic nodules: an uncommon case during
cesarean section. Pan Afr Med J. 2019;34:7.
12. Pekin A, Ozaydin I,
Hakverdi AU. Diffuse ectopic deciduosis imitating peritoneal carcinomatosis
with acute abdomen syndrome—case report and literature review. Case Rep Obstet
Gynecol. 2020;2020:7533791.
13. Buttner A, Bohnert M,
Sperhake J, Tsokos M. Ectopic decidua: diagnostic pitfalls. Forensic Sci Int.
2013;233(1-3):e13–e18.
14. Buttner A, Tsokos M.
Florid diffuse peritoneal deciduosis mimicking carcinomatosis in a twin
pregnancy case report. Case Rep Pathol. 2013;2013:3816836.
15. Zaystev A, Sopilnyak N,
Boyko K, et al. Ectopic decidua: Pathogenesis and clinical implications. J Clin
Pathol. 2021;74(12):789-794.
16. Galão AO, Ramos LF,
Schuh F, Golbspan L, Grezzana TJ. Ectopic decidua in pregnancy discovered
incidentally during caesarean delivery. Journal of Obstetrics and Gynaecolog.
201;33(2), 207–208.
17. Garrido T, Dominguez F,
Quiñonero A, Diaz-Gimeno P, Kapidzic M, Gormley, et al. Defective
decidualization during and after severe preeclampsia reveals a possible
maternal contribution to the etiology. Proc. Natl. Acad. Sci. 2017;E8468-E8477.
18. Attanoos RL, Gibbs AR.
Mesothelioma and related diseases. Diagn Histopathol. 2011;17(6):253-260.
19. Vyskharenko AL, Liakina
TL, Zadorozhna MV. Differential diagnosis of metastatic melanoma and other
tumors in unusual locations. Int J Clin Exp Pathol. 2017;10(9):9656-9662.
20. Sorokin P, Nikiforchin
A, Panin A, Zhukov A, Gushchin V, Kurtser M. Diffuse Ectopic Deciduosis
Imitating Peritoneal Carcinomatosis with Acute Abdomen Presentation: A Case
Report and Literature Review. Case Rep Obstet Gynecol. 2020;2020:8847082.