The burden of care
and its correlates in family caregivers of breast cancer patients undergoing chemotherapy
in Sari, Iran, in 2020
Mehrooz Alishah 1, Masoumeh Bagheri-Nesami 2,3,
Seyed Robabe Babaei 1*, Jamshid Yazdani-Cherati 4, Mehrnoosh Alishah 5
1 Nasibeh School of Nursing and
Midwifery, Mazandaran University of Medical Sciences, Sari, Iran
2 Traditional and Complementary
Medicine Research Center, Addiction Institute, Mazandaran University of Medical
Sciences, Sari, Iran
3 World Federation of
Acupuncture-Moxibustion Societies (WFAS), Beijing, China
4 Health Sciences Research Center,
Mazandaran University of Medical Sciences, Sari, Iran
5 Information Science, Mazandaran
University of Medical Sciences, Sari, Iran
*Corresponding
Author: Seyed Robabe Babaei
* Email: robabe.babaei@gmail.com
Abstract
Introduction: Caring for patients with cancer can often give rise to numerous
physical and mental health problems or even exacerbate them among family
caregivers. The present study aimed to reflect on the burden of care and its
correlates affecting family caregivers of breast cancer (BC) patients
undergoing chemotherapy.
Materials and Methods: This descriptive-analytical cross-sectional study of correlational
type was conducted on a total number of 163 family caregivers of patients with
BC undergoing chemotherapy at Imam Khomeini Teaching Hospital and Baghban
Specialized Center based in the city of Sari, Iran, in 2020. For this purpose,
the study samples were selected through the available sampling technique. As
well, the demographic characteristics information form and the Caregiver Burden
Inventory (CBI) were employed for data collection. The data were ultimately
analyzed using the SPSS Statistics software (ver. 21).
Results: The study results revealed that 72 family caregivers (44.17%) were
experiencing high levels of burden of care (>36). Moreover, caregivers’
level of income, number of chemotherapy sessions, duration of disease, and
patients’ insurance coverage status were significantly correlated with
caregiver burden, which were evaluated in the multiple logistic regression
analysis. This model could further explain 25.2% of variance in the burden of
care severity in these informal caregivers (p<0.001, Chi-square [χ2]
statistic=33.9). The multiple logistic regression analysis was also utilized to
determine the effect of the most important dimensions of the burden of care and
this model could account for 94.8% of variance in the burden of care severity among
these family caregivers, wherein developmental, social, physical, and time
dependence dimensions respectively had the greatest impacts on compounding
caregiver burden.
Conclusion: The study results indicated high levels of burden of care in family
caregivers of patients suffering from BC. Therefore, it was recommended to
consider the burden of care correlates and to plan for proper interventions,
according to the findings in the present study, in further research.
Keywords: Burden of Care, Breast Cancer, Demographic Characteristics, Patient
Companion
Introduction
Cancer
is known as one of the most important diseases in the 21st century (1), so a
significant share of health care programs has been allocated to this condition
(2). Asia also has the highest prevalence rate of cancer (48% of the cases over
the world) among all continents. In this respect, 1 out of every 8-10 women
across the world and 1 out of every 10-15 women in Iran, have a higher chance
of developing breast cancer (BC) (3). As well, this type of cancer in Iran
accounts for 21.4% of all reported cases (4). The incidence of this condition
in this country, particularly in central and Northern provinces is considerably
on the increase (5). The onset age of developing BC in Iran is also one decade
lower than that in Western countries (6). This disease can thus affect various
aspects of life in women. Diagnostic tests and medical procedures,
complications induced by treatments such as nutritional problems, fatigue,
nausea, vomiting, and pain, as well as disruptions of social relationships and
care/treatment costs are among other consequences of this condition (7). Given
the debilitating nature of cancer and its related care/treatment, most of those
suffering from this disease need more support by informal caregivers (1), who
might have a sense of despair, loneliness, and failure in assuming their own
duties due to no education with regard to the disease and receiving no
information support in this domain (8). As 55% of care is provided by informal
caregivers, such people mostly fail to meet their own needs in daily living and
even ignore them to provide care for their loved ones (9). The mean time of
care for cancer patients has been estimated by 8.8 hours per day (10) and
family caregivers are required to fulfill not only their daily routine
activities but also their obligations in the workplace (11). Under such
conditions, if family caregivers fail to manage the time of care for patients
and that allocated to their own personal issues, they will progress towards the
burden of care (10). Here, caregiver burden is a general term to describe
physical, emotional, and socioeconomic costs of care. It has been also defined
as the product of the imbalance between costs of patient care and those for
care facilities (12). Although the caring role in caregivers can raise a sense
of affection and love in these individuals and bring some benefits such as a
meaningful life, more intimacy in family relationships, respect for oneself and
others, as well as a sense of satisfaction (13),
it might be accompanied by problems such as burnout, anxiety,
depression, insomnia, decreased appetite, and hypertension (14, 15). Studies
have further shown that factors such as duration of care, family economic
status, social support, number of caregivers, type of disease, increased
duration of disease, and clinical symptoms in patients can have significant
effects on the burden of care (16, 17). Given the high importance of caregivers
in support of patients to deal with BC and considering the growing population
with this condition and little research on the burden of care, this study aimed
to evaluate the burden of care and its correlates in family caregivers of
patients with BC undergoing chemotherapy.
Materials and Methods
This descriptive-analytical cross-sectional study of correlational
type was conducted in the chemotherapy wards of Imam Khomeini Teaching Hospital
and Baghban Specialized Center based in the city of Sari, Iran, in 2020. The
statistical population included all caregivers of BC patients referred to these
centers, of which 163 caregivers of the patients undergoing chemotherapy were
selected.
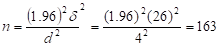
The sample size was further estimated to be 163 individuals based
on the study by Adili and Dehghan Araie (18), using the following calculation
formula:
Of note, this
research project was approved by the Research Ethics Committee of Mazandaran
University of Medical Sciences, Sari, Iran (IR.MAZUMS.REC.1399.6442). During 11
months (from April to January 2020), the convenience sampling technique was
performed after providing explanations and obtaining written consent from the
family caregivers. Ethical considerations in this study were also met by
observing the confidentiality of information, voluntary participation in the
research, possibility of withdrawing from the project without time
restrictions, and explaining the objectives and the research procedure to the
study samples.
The primary family caregivers of the patients included spouse,
sibling, and parent. As well, the inclusion criteria were literacy (i.e.,
reading and writing ability), age over 18 years, no mental illnesses, and
approvals that these individuals were the primary caregivers and companions.
Moreover, those receiving counseling and psychology services, taking sedatives
and tranquilizers, or caring for patients with underlying diseases or the ones
with metastatic progression were excluded.
 The data in
this study were collected using two-part questionnaire. The first part
contained the demographic characteristics information form about the family
caregivers (including gender, age, marital status, level of education,
occupation, and kinship) and the patients (such as gender, age, marital status,
level of education, occupation, housing, level of income, duration of disease,
insurance coverage status, and number of chemotherapy sessions).
The data in
this study were collected using two-part questionnaire. The first part
contained the demographic characteristics information form about the family
caregivers (including gender, age, marital status, level of education,
occupation, and kinship) and the patients (such as gender, age, marital status,
level of education, occupation, housing, level of income, duration of disease,
insurance coverage status, and number of chemotherapy sessions).
The second part of the questionnaire was the 24-item Caregiver
Burden Inventory (CBI), developed by Novak and Guest (1989), which was utilized
to evaluate the level of burden of care perceived by the caregivers in an
objective and subjective manner. This questionnaire measured the burden of care
in five dimensions, i.e., time dependence, developmental, physical, social, and
emotional (18). The total score could be also from zero to 96, in which scores
of <35 indicated lower level of burden of care and the scores of ≥36
represented higher levels of burden of care. The participants could further
determine the degree of their experiences with each situation in a five-point
Likert-type scale - completely false (0 point) false (1 point), to some extent
(2 points), true (3 points), and completely true (4 points).
The CBI was translated by Abbasi et al. into Persian and its
validity was further confirmed through content validity method. In a study on
patients with end-stage cancer, the Cronbach’s alpha coefficient had been
similarly calculated by 0.90 (2). In order to analyze the data, they were
firstly summarized using descriptive statistics including mean and standard
deviation (SD) for the quantitative data and frequency tables for the
qualitative ones. Then, descriptive statistics, independent-samples t-test,
Chi-square test, and Spearman’s rank-order correlation were employed to examine
the relationships. The final analysis of the relationships was done through the
multiple logistic regression analysis at a significance level of 0.05, using
the SPSS Statistics software (Ver. 24). After the normality of data was
examined, the Kolmogorov-Smirnov test was used for inferential analysis.
Results
A total number of 163 primary family caregivers, most of them as
the spouse of 85 patients (52.1%), with a mean age of 43.6±11.7 years were
studied. The results also revealed that 55.83% and 44.17% of the family
caregivers had low and high levels of burden of care, respectively. Given the
demographic characteristics information, most of the family caregivers in this
study were male caregivers (n=97, 59.5%), married individuals (n=136, 83.4%),
those holding university degrees (n=66, 40.5%), homemakers (n=45, 27.6%), the
ones owning a house (n=132, 81%) and cases with a moderate-to-high level of
income (n=129, 79.2%). According to the demographic characteristics of the
patients, majority of them in this study were married (n=141, 86.5%), had high
school diploma and lower degrees (n=118, 72.4%), owned a house (n=128, 78.5%),
and a moderate level of income (n=77, 47.2%) as well as insurance coverage
(n=150, 92%). Of these patients, 149 cases (91.4%) also had
chemotherapy-induced complications (Table 1). The mean age of the patients in
this study was 46.7±10.6 years old, the mean length of chemotherapy was
6.26±4.3 sessions, and the mean duration of disease from diagnosis was 7.86±6.7
months.
The logistic regression analysis was further used to determine the
correlates affecting the burden of care in family caregivers. First, the
univariate mode of the logistic regression analysis was implemented and the
variables whose values were <0.3 were selected for the multiple logistic
regression model. Next, employing the multivariate logistic regression analysis
and the backward stepwise selection method, the given variables were considered
for the model with the probability of excluding each variable by 0.1. The
variables of the family caregivers’ level of education, occupation, level of
income, and kinship along with the patients’ marital status, occupation, level
of income, number of chemotherapy sessions, chemotherapy-induced complications,
duration of disease, and insurance coverage status whose univariate p-values
were <0.3 were also taken into consideration for the final model of the
multiple logistic regression analysis. Within the final model, the four
variables of family caregivers’ level of income as well as number of
chemotherapy sessions, duration of disease, and patients’ insurance coverage
status remained.
Discussion
This study aimed to evaluate the burden of care and its correlates
in family caregivers of BC patients undergoing chemotherapy. The results showed
that almost half of these informal caregivers (44.17%) had experienced high
levels of burden of care (>36), which was lower compared with the findings
in Salmani et al. (20) who had reported the burden of care in Iranian caregivers
of patients admitted to the oncology ward by 81% and in the survey by Gabriel
(21) in which the burden of care in the primary caregivers of the patients with
BC in Nigeria had been 86.7%. It seems that the metastasis and the underlying
conditions could be the main reasons for this discrepancy. It should be noted
that the patients in the present study were undergoing chemotherapy, the exclusion
criteria were metastatic BC and underlying diseases. In the survey on the
patients with advanced cancer, living in Northern England, Higginson (22) had
also found that the patient caregivers were experiencing a lower level of
burden of care (18.5±11). The researchers had attributed such findings to
receiving domestic support services to the caregivers (23). In any case, cancer
might put too much mental strain on family members, especially patients’
spouses, and the evidence shows that they suffer from the highest levels of
burden of care (24) because they are closer to their own patients with regard
to emotional and physiological problems and feel more responsible in caring for
their patients, which can produce greater levels of burden of care among them.
In the present study, the higher the caregivers’ level of income,
the lower the level of burden of care, which was consistent with the reported
results by Gabriel (21) and Vahidi (25), examining the burden of care among the
caregivers of BC patients. They also highlighted the relationship between the
low level of income and the increased level of burden of care. Some studies had
similarly demonstrated a significant correlation between economic status and
low level of income and higher level of burden of care (26- 28). These findings
were additionally observed in the research by Hanratty, wherein most caregivers
had to quit their jobs to provide full-time care to their patients, leading to
further financial problems as well as elevated level of burden of care (29). As
a result, more support for low-income caregivers to reduce the levels of burden
of care seems necessary.
Besides, this study showed that a rising trend in the number of
chemotherapy sessions could produce the burden of care. Given that weakness and
disability increase in patients during chemotherapy sessions and the patients
might be subjected to new complications at the end of each session, this issue
leads to higher level of burden of care among caregivers.
The results of this study suggested that the burden of care reduced
as the disease prolonged from diagnosis to treatment. In conflict with the
present study, Germain et al. researched the burden of care in the elderly
patients with cancer (30). The age of the patients in both studies could be the
reason for the different results because older adults might demand more care.
On the other hand, the patients in the present study were young or middle-aged,
so they could gradually perform many diagnostic tests before treatment on their
own, and they needed no constant caregivers.
The study results indicated that the caregivers whose patients were
benefiting more support from insurance services had lower levels of burden of
care, which was in line with the survey by Hu and Peng (31) on the burden of
care in caregivers of patients with lung cancer and the findings by Johnson
(32) on the burden of care among caregivers of oncology patients receiving
chemotherapy. In these studies, the insurance coverage status and social
support had been reported as the factors affecting the burden of care in the
caregivers. It seems that the role of authorities committing insurance caregivers
to provide medications for these patients has a significant impact on
minimizing the level of burden of care. The results of the present study were
not in agreement with the reports by Adili (18), exploring the relationship
between the burden of care and the patients’ quality of life in caregivers of
BC patients. The reason for this discrepancy could be in the time of diagnosis,
which was only three months in the survey by Adili, when it seems that the
financial resources in family could still meet the financial needs of the
patients. In the present study, however, this time was longer.
Since family caregivers must meet their own needs and those of
patients, they suffer from additional levels of burden of care in all physical,
emotional, and socioeconomic aspects along with disruption in their caring
roles (33). This study showed that the most frequent burden of care among the primary
caregivers was related to developmental, social, physical, and time dependence
dimensions, which was in line with the survey by Ghane et al. (34), reporting
the developmental burden of care as the most common dimension in the family
caregivers of patients undergoing hemodialysis. However, Abbasi et al. (35) had
mentioned the most frequent burden associated with the emotional dimension of
care for patients receiving hemodialysis. In a study on colorectal cancer (CRC)
patients, Bakim (36) had revealed that aging could lead to higher levels of
burden of care in the caregivers. Since the increase in age in the caregivers
reduces the emotional dimension of the burden of care following gaining
experience (37) and a rise in physical, developmental, and time dependence
dimensions (35), this can be justified with regard to the mean age of the
caregivers (46.7±10.6 years old). Unsar et al. (38) had also indicated that the
caregivers of cancer patients had to care for them all day long, so they had no
spare time for themselves. Employment outside the home could similarly create
an elevated level of burden of care due to the conflict between work and caring
responsibilities (28). As well, Shafie Zadeh et al. (39), investigating the
relationship between the burden of care and the demographic characteristics of
the caregivers of the elderly with Alzheimer’s disease, had found that these caregivers
had experienced the maximum level of burden of care related to the time
dependence dimension. It seems that the duration of care for such patients,
depending on the type of the disease, can be a factor affecting the burden of
care severity as the Alzheimer’s disease needs constant care, while in this
study, the patients did not demand full-time care according to the caregivers.
At the end of the questionnaire and according to the survey
conducted among the caregivers to offer their suggestions with regard to the
burden of care, financial and insurance support especially for the provision of
medications and information on how to take care and deal with the complications
in the patients were among the issues noted by most of the caregivers. Studies
have further shown an inverse relationship between the burden of care and
social support (40, 41). In other words, caregivers may have more time and
energy to care for oneself and to meet their own needs whenever they take
advantage of higher levels of social support from family and professional
institutions.
It seems that the use of different sampling techniques, variations
in receiving care services, support services, cultural discrepancies, types of
organizations involved in cancer care/treatment, as well as the most recent
breakthroughs in BC care/treatment can be among the reasons for inconsistencies
in the results of such studies.
Since this study was conducted during the coronavirus disease 2019
(COVID-19) pandemic and some caregivers were reluctant to complete the
questionnaires manually, a number of the questionnaires were unavoidably done
through interviews, which could increase the possibility of unreal responses by
them. It was also possible that the caregivers tended not to talk about the
burden of care or underestimate it, and even feel guilty to tell the truth in
this regard.
Conclusion
The study results revealed that the caregivers of the BC patients
were suffering from the burden of care during chemotherapy. Based on the study
findings, caregivers’ level of income, number of chemotherapy sessions,
duration of disease, and insurance coverage status are significantly correlated
with their burden of care. The correlation between some demographic
characteristics information and the burden of care among the caregivers of this
category of patients is further highlighted. Accordingly, information is
provided in order to improve the existing situation of the caregivers and to
reduce the burden of care. If the caregivers’ burden of care is mitigated, they
can play their caring roles better. Given the results of the present study,
there is a need to reflect more on the caregivers’ developmental and social
dimensions of the burden of care. It is also recommended to provide nurses with
the outcomes of the most recent studies on caring for cancer patients in the
form of training courses to help them meet the educational needs of informal
caregivers in order not to feel frustrated and isolated. Caregivers must be
also supported by health care providers and a person should be always available
as a supporter to respond to the questions posed by these caregivers and help
them have lower burden of care. Health care team members should remember that
the main respondents to cancer patients are their primary caregivers, whose
value should never be overlooked in the health care team. Technology resources
including telephone follow-up, virtual care guide, and online support groups
can be thus effective in these conditions.
Author contributions
MA, MBN, JYCh and MA wrote and
completed the article. SRB designed and edited the manuscript. All authors confirmed the final edited
version.
Acknowledgments
The authors hereby extend their gratitude to the honorable
officials for their collaboration, as well as the financial support granted by
the Vice Chancellor’s Office for Research at Mazandaran University of Medical
Sciences, Sari, Iran (IR.MAZUMS.REC.1399.6442). They also appreciate the
caregivers of the patients referring to Imam Khomeini Teaching Hospital and Baghban
Specialized Center, Sari, Iran, along with all nurses who provided the grounds
for the completion of this research project.
Conflicts of interest
There are no conflicts of interest.
References
1. OHara RE, Hull JG, Lyons KD, Bakitas M, Hegel MT,
Li Z, et al. Impact on caregiver burden of a patient-focused palliative care
intervention for patients with advanced cancer. Palliative & supportive
care. 2010;8(4):395-404.
2. Rajabi M, Bastami M, Shahvaroughi Farahani N,
Tavanaie A, Ghanbari B, Alasti H. Religious Coping as a Predictor of the Burden
of Care in the Caregivers of End-stage Cancer Patients. Iran Journal of
Nursing. 2018;31(114):6-16.
3. Kazemzadeh S, Babaei E.
Investigating the expression of CCAT2 gene as a new molecular marker in breast
tumors. Journal of Fasa University of Medical Sciences. 2018;7(4):573-81.
4. Akinyemiju TF. Socio-economic and health access
determinants of breast and cervical cancer screening in low-income countries: analysis of the World Health Survey. PloS one. 2012;7(11): 34-48.
5.Enayatrad M, Salehiniya H. An investigation of
changing patterns in breast cancer incidence trends among Iranian women. J
Sabzevar Univ Med Sci. 2015;22(1):27-35.
6. Fazeli Z, Najafian ZM, Eshrati B, ALMASI HA.
Five-year evaluation of epidemiological, geographical distribution and survival
analysis of breast cancer in Markazi Province, 2007-11. 2014.
7. Hatami H, Azizi F, Janghorbani M. Epidemiology
and control of common disorders in Iran. Tehran, Iran: Khosravi Publications.
2004.
8. Mashayekhi F, Pilevarzadeh M, Rafati F. The
assessment of caregiver burden in caregivers of hemodialysis patients. Materia
socio-medica. 2015;27(5):333.
9. Nijboer C, Tempelaar R, Sanderman R, Triemstra M, Spruijt RJ, Van Den Bos GA. Cancer and caregiving: the impact on the
caregiver's health. Psycho‐Oncology: Journal of the Psychological, Social and
Behavioral Dimensions of Cancer. 1998;7(1):3-13.
10. Girgis A, Lambert S, Johnson C, Waller A,
Currow D. Physical, psychosocial, relationship, and economic burden of caring
for people with cancer: a review. Journal of Oncology Practice.
2012;9(4):197-202.
11. Khatti Dizabadi F,
Yazdani J, Eftekhar Ardebili H, Batebi A, Shojaezadeh D. The status of
caregiving among informal caregivers of community-dwelling elderly. Journal of
Mazandaran University of Medical Sciences. 2013;23(100):31-41.
12. Govina O, Kotronoulas G,
Mystakidou K, Katsaragakis S, Vlachou E, Patiraki E. Effects of patient and
personal demographic, clinical and psychosocial characteristics on the
burden of family members caring for patients with advanced cancer in Greece.
European Journal of Oncology Nursing. 2015;19(1):81-8.
13. Alnazly EK. Burden and coping strategies among
J ordanian caregivers of patients undergoing hemodialysis. Hemodialysis
International. 2016;20(1):84-93.
14. Ardeshirzadeh M.
Comparative study of psychological burden in caregivers of chronic
schizophrenic and bipolar patients; coping approaches. research based final
theses, University of Welfare and Rehabilitation Sciences. 2004.
15. Chindaprasirt J, Limpawattana P, Pakkaratho P,
Wirasorn K, Sookprasert A, Kongbunkiat K, et al. Burdens among caregivers of
older adults with advanced cancer and risk factors. Asian Pac J Cancer Prev. 2014;15(4):1643-8.
16. Kahriman F, Zaybak A.
Caregiver burden and perceived social support among caregivers of patients with
cancer. Asian Pac J Cancer Prev. 2015;16(8):3313-7.
17. Choi YS, Hwang SW, Hwang IC, Lee YJ, Kim YS,
Kim HM, et al. Factors associated with quality of life among family caregivers
of terminally ill cancer patients. Psycho‐Oncology. 2016;25(2):217-24.
18. Adili D, Dehghani-Arani
F. The relationship between caregiver's burden and patient's quality of life in
women with breast cancer. Journal of Research in Psychological Health.
2018;10(2):30-9.
19. Novak M, Guest C. Application of a
multidimensional caregiver burden inventory. The gerontologist.
1989;29(6):798-803.
20. Salmani N, Ashktrab T, Hassanvand S. Care stress
and its related factors in caregivers of patients in the oncology ward of Shah
Vali Hospital, Yazd, Journal of the School of Nursing and
Midwifery.2014;24(84):11-17.
21. Gabriel I, Aluko J, Okeme M. Caregiver burden
among informal caregivers of women with breast cancer. Biomed J Sci Tech.
2019;15:1-9.
22. Higginson IJ, Gao W. Caregiver assessment of
patients with advanced cancer: concordance with patients, effect of burden and
positivity. Health and quality of life outcomes. 2008;6(1):1-8.
23. Seven M, Yılmaz S, Şahin E, Akyüz A.
Evaluation of the quality of life of caregivers in gynecological cancer
patients. Journal of Cancer Education. 2014;29(2):325-32.
24. Bigatti SM, Brown LF, Steiner JL, Miller KD.
Breast cancer in a wife: How husbands cope and how well it works. Cancer
Nursing. 2011 May 1;34(3):193-201.
25. Vahidi M, Mahdavi N, Asghari E, Ebrahimi H,
Ziaei JE, Hosseinzadeh M, et al. Other side of breast cancer: Factors
associated with caregiver burden. Asian nursing research. 2016;10(3):201-6.
26. Cormac I, Tihanyi P. Meeting the mental and
physical healthcare needs of carers. Advances in Psychiatric Treatment.
2006;12(3):162-72.
27. Yoon S-J, Kim J-S, Jung J-G, Kim S-S, Kim S.
Modifiable factors associated with caregiver burden among family caregivers of
terminally ill Korean cancer patients. Supportive Care in Cancer.
2014;22(5):1243-50.
28. Hsu T, Loscalzo M, Ramani
R, Forman S, Popplewell L, Clark K, et al. Factors associated with high burden
in caregivers of older adults with cancer. Cancer. 2014;120(18):2927-35.
29. Hanratty B, Holland P, Jacoby A, Whitehead M.
Financial stress and strain associated with terminal cancer—a review of the
evidence. Palliative Medicine. 2007;21(7):595-607.
30. Germain V, Dabakuyo-Yonli TS, Marilier S,
Putot A, Bengrine-Lefevre L, Arveux P, et al. Management of elderly patients
suffering from cancer: Assessment of perceived burden and of quality of life of
primary caregivers. Journal of geriatric oncology. 2017;8(3):220-8.
31. Hu X, Peng X, Su Y, Huang
W. Caregiver burden among Chinese family caregivers of patients with lung cancer: a cross-sectional
survey. European journal of oncology nursing. 2018;37:74-80.
32. Johansen S, Cvancarova M,
Ruland C. The effect of cancer patients’ and their family caregivers’ physical
and emotional symptoms on caregiver burden. Cancer Nursing. 2018;41(2):91-9.
33. Bayoumi MM. Subjective burden on family carers
of hemodialysis patients. Open Journal of Nephrology. 2014;4(2):89-96.
34. Ghane G, Ashghali Farahani M, Naime SF, Haqqani H,
et al. The effect of supportive education program on the care pressure of
family caregivers of patients undergoing hemodialysis. Journal of Nursing and
Midwifery. 2017; 14 (10): 885-95.
35. Abbasi A, Ashrafrezaee N, Asayesh H, Shariati A,
Rahmani H, Mollaei E, et al . The Relationship Between Caring Burden And Coping
Strategies In Hemodialysis Patients Caregivers. Journal of research development
in nursing and Midwifery Fac. 2011; 8 (1):26-33.
36. Bakım KKHBV. Assessment of the caregiver
burden of caregivers of colorectal cancer patients. Turk J Colorectal Dis.
2018;28:164-71.
37. Mollaoğlu M, Kayataş M, Yürügen B. Effects on
caregiver burden of education related to home care in patients undergoing
hemodialysis. Hemodialysis International. 2013;17(3):413-20.
38. Unsar S, Erol O, Ozdemir O. Caregiving burden,
depression, and anxiety in family caregivers of patients with cancer. European
Journal of Oncology Nursing. 2021;50:101882.
39. Shafizadeh Kholanjani A, Mirzaei A, Heravi
Karimovi M, Parade Sharifnia S.H, Montazeri A. Relationship between caring
burden and demographic characteristics of caregivers of the elderly with
Alzheimer's disease. Journal of Nursing Education. 2020 Mar 10; 9 (1): 65-73.
40. Maheshwari Preksha S,
Kaur M. Perceived social support and burden among family caregivers of cancer
patients. Int J Health Sci Res. 2016;6(1):304-14.
41. Nightingale CL, Curbow BA, Wingard JR, Pereira
DB, Carnaby GD. Burden, quality of life, and social support in caregivers of
patients undergoing radiotherapy for head and neck cancer: A pilot study.
Chronic illness. 2016;12(3):236-45.
![]()
![]() The data in
this study were collected using two-part questionnaire. The first part
contained the demographic characteristics information form about the family
caregivers (including gender, age, marital status, level of education,
occupation, and kinship) and the patients (such as gender, age, marital status,
level of education, occupation, housing, level of income, duration of disease,
insurance coverage status, and number of chemotherapy sessions).
The data in
this study were collected using two-part questionnaire. The first part
contained the demographic characteristics information form about the family
caregivers (including gender, age, marital status, level of education,
occupation, and kinship) and the patients (such as gender, age, marital status,
level of education, occupation, housing, level of income, duration of disease,
insurance coverage status, and number of chemotherapy sessions).