Investigation of
self-harm cases and related factors
Morteza Rahbar Taramsari 1*, Ardeshir Sheikh-Azadi 2
1 Department of Forensic Medicine,
School of Medicine, Guilan University of Medical Sciences, Rasht, Iran
2 Department of Anatomy, School of
Medicine, Alborz University of Medical Sciences, Karaj, Iran
*Corresponding
Author: Morteza Rahbar Taramsari
* Email: rahbar_m46@yahoo.com
Abstract
Introduction:
Self-harm
is a deliberate and non-lethal act in which a person intentionally injures
himself or consumes a substance in excess of the prescribed amount. Self-harm
injuries are also seen in forensic clients. Self-mutilation in these people is
done in order to achieve a goal and is accompanied by claims of delusion of
others. The importance of this issue is the necessary urgency in
differentiating it from suicide, malice, mock disease and conversion diseases.
In this study, we have examined self-harm and some related factors.
Materials
and Methods: In a retrospective cross-sectional descriptive study, a checklist
including two sections of demographic information and self-harm information was
prepared to collect the necessary information based on a review of the texts
and was completed by the researcher for each case. The obtained data were
analyzed using descriptive tests of SPSS statistical software.
Results:
Out
of 783 cases, 467 (59.6%) were men and the mean age of 783 patients was 28.25 ±
8.38 years. A higher percentage of clients had more lesions on the left side of
their body (61.4%), referred with a scratch lesion (46.0%), referred to a
lesion in the arm area (25.7%) and of hard-edged objects used for self-harm.
Conclusion:
In
the face of someone who self-harms, two things should be considered, one is to
achieve an appropriate treatment path considering the possibility of a mental
illness that is more relevant to hospital physicians and the second is a legal
view of this. From the perspective of forensic science to differentiate the
damage caused by conflict and self-harm.
Keywords:
Self-harm,
Forensics, Aggression
Introduction
Aggression is defined as behavior that
aims to harm oneself or another. Aggression in humans represents the instinct
of death as opposed to the instinct of life in action. This instinct destroys
others if it can, and if it fails to target others aggressively, it will turn
to itself and manifest itself as self-harm and suicide (1).
Compared to suicide, self-harm is done to change current emotions, but suicide
is done to end current emotions. People who self-harm are usually considered
unpopular and problematic, difficult to tolerate, and many of whom have severe
social and personal problems and need care (2). Self-harm is a deliberate and non-lethal act
in which a person intentionally injures himself or herself in various forms
such as poisoning (drugs, alcohol, etc.), interfering with wound healing,
jumping from a height, interfering with wound healing, or shooting himself (3).
Self-harmers cite a wide range of causes for self-harm, including energy gain,
addiction, body control, sexual pleasure, and uniqueness (4).
Self-harm injuries are also seen in
forensic clients. Self-mutilation in these people is done to achieve a goal and
is accompanied by claims of delusion of others. On the other hand, motivations
in self-harming people were classified into 4 groups, which were in the form of
involuntary negative reinforcement (stopping bad feelings), involuntary positive
reinforcement (self-punishment), negative social reinforcement (not going to
work) and positive social reinforcement (Draw attention) (5). The prevalence of self-harm is higher
in early adulthood and can be the first manifestation of a mental illness. It
is also more common in people with a history of child sexual abuse (6). Alcohol and substance abuse are more
common in these people, and a higher percentage of these people have long-term
mental health problems. The younger the age of onset of self-harm, the more
unfavorable the prognosis and the longer and longer periods and the variety of
self-harm methods (7). Today, with the advancement of
genetics, theories have been proposed to indicate the relationship between
specific genetic patterns and psychiatric disorders (8). In this study, we have examined
self-harm and some related factors.
Materials and Methods
In a retrospective cross-sectional descriptive
study, 783 patients were examined for self-harm. To collect the necessary
information based on the review of the texts, the checklist includes two
sections of demographic information (age, sex, marital status, occupation,
education, history of alcohol and smoking, history of suicide and previous
self-mutilation, presence of tattoos) and information related to Self-harm
(location of injury, side of injury, number of injuries, impact device and
number of lesions) was prepared and completed by the researcher for each case.
The data were analyzed using descriptive tests of SPSS statistical software.
Continuous variables were presented as mean ± SD and
discrete data as frequency percentage.
Out of 783 clients due to self-harm, 467
(59.6%) were men and the mean age of 783 patients was 28.25 ± 8.38 years, while
the youngest was 16 years old and the oldest was 60 years old.
Most forensic clients who had
self-harmed were unemployed (45.5%), with a diploma-postgraduate degree
(37.2%), married (50.6%), right-handed, with more lesions on the left side of
their body. (61.4%), no previous history of self-harm (65.4%), no history of
mental illness (76.4%), no history of suicide (0.93%), no tattoos on body
surfaces (81.5%) 3), no alcohol consumption (75.7%), no smoking (65.3%). The
frequency of scratch lesions (46%) was higher than bruises, abrasions,
scratches, cuts, tears and burns. The highest frequency distribution of lesions
with lesions was in the arm area (25.7%), followed by lesions in the forearm area
(19.9%) and then lesions in the neck area (15.3%) (Table 1). A higher
percentage of clients presented with a lesion (64.7%) (Figure 1).
Table 1. Frequency distribution of the lesions
area created by self-harming individuals.
|
The location of the
lesion |
face |
Neck |
Arm |
Forearm |
Front of the body |
Back of the body |
Thigh |
Leg |
Total |
|
Number |
35 |
120 |
201 |
156 |
125 |
70 |
41 |
35 |
783 |
|
Percent |
4.5 |
15.3 |
25.7 |
19.9 |
16. |
8.9 |
5.2 |
4.5 |
100 |
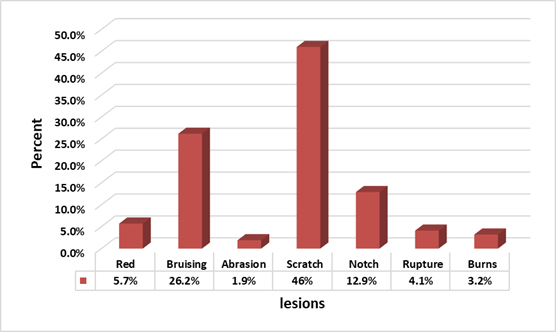
Figure 1. Frequency distribution of lesions
generated by self-harmers.