Impact of induction chemotherapy on resectability of borderline resectable/unresectable oral cavity carcinomas
Induction chemotherapy in borderline resectable oral cavity cancers
Keywords:
Neoadjuvant chemotherapy, Borderline resectable, Unresectable, Oral cavity cancer, Overall survivalAbstract
Introduction: To assess the impact of neoadjuvant chemotherapy (NACT) on achieving surgical resectability in patients with borderline resectable or unresectable T4a oral cavity squamous cell carcinoma (OCSCC).
Materials and methods: Patients with borderline resectable or unresectable T4a OCSCC enrolled between October 2023 and June 2025 received three to four cycles of NACT. Post-treatment, patients were assessed for response and resectability using clinical and radiological criteria.
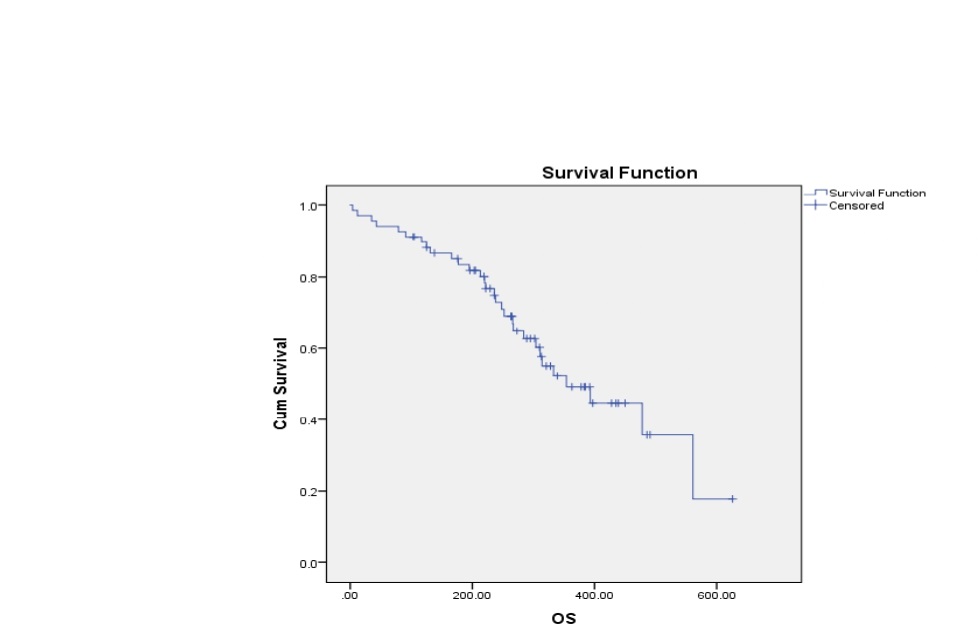
Results: A total of 102 patients received NACT; 65.7% were male (n = 67) and 34.3% were female (n = 35). The median age was 47 years (range: 28–72). All patients received either two-weekly or three-weekly TPF regimens. Tobacco use and combined alcohol–tobacco habits were the most common (44.1% each), followed by tobacco with betel nut (4.9%), betel nut alone (2.9%), and no habits (3.9%). The buccal mucosa was the most frequent primary site (41.1%), followed by the tongue (35.2%). Other sites included the retromolar trigone (8.9%), upper alveolus (6.8%), and gingivobuccal sulcus (6.8%). Most patients presented with cT4aN1 disease (30.3%).The two-weekly TPF regimen was more commonly used (58.8%) than the three-weekly regimen (41.1%). Toxicity was manageable, with 36.3% of patients experiencing no adverse effects. The most frequent response was partial response (39.2%), followed by progressive disease and unevaluable responses (23.5% each), stable disease (8.8%), and complete response (4.9%). Surgery was considered feasible in 33 patients (32.3%), and 25 (24.5%) ultimately underwent surgery. Patients who underwent surgery demonstrated a significantly improved median overall survival (17.4 months) compared with those managed non-surgically (10.2 months; log-rank p = 0.001).
Conclusion: NACT is well tolerated and has an acceptable toxicity profile, enabling conversion to resectability in nearly one-third of patients with borderline resectable or unresectable T4a OCSCC. Surgical intervention significantly improves overall survival, underscoring the potential role of NACT in appropriately selected patients.
Published
How to Cite
License
Copyright (c) 2025 L.K. Rajeev , Dayananda Sagar P, K.N. Lokesh, Chetan V, A.H. Rudresh, G.V. Giri, Smitha C Saldanha, Yaman Patidar, Suresh Babu

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.